The following is adapted from a case presented in the New England
Journal of Medicine.
New England Journal of Medicine (2019) "Weak and Winded" 381:
76-82. Quotes from the text of the paper are presented in
the yellow blocks; questions are presented in the blue blocks.
A 22-year-old woman with a history of sickle cell disease and migraine headaches presented to the emergency department with weakness that had caused her to fall that day. She reported a gradual progression of weakness over a period of 6 months, which had lead in the previous few weeks to difficulty standing, climbing steps, and lifting her child. Her weakness was symmetric in both her arms and her legs...She reported no cognitive impairment, paresthesia, numbness, or urinary incontinence.
There are many possible causes for muscle weakness. Potential causes are:
What is meant by the term "paresthesia"?
Which of the above problems would cause paresthesias?
This patient shows no cognitive impairment or issues with bladder control suggesting that her weakness is unlikely to be due to a problem in the central nervous system. Furthermore, the gradual onset of symptoms argues against stroke as a cause of her weakness. The lack of sensory symptoms (numbness or paresthesia) also makes peripheral neuropathy unlikely.
The patient had had intermittent choking episodes and difficulty swallowing over the previous 2 months, but reported no difficulty chewing.
She also reported shortness of breath with minimal
exertion...Computed tomographic (CT) angiography of the chest
[was] normal...Chest radiography showed no acute cardiopulmonary
process. Results of CT, with contrast, of the chest,
abdomen, and pelvis were normal.
Dyspnea is the medical term for shortness of breath. Dyspnea might be caused by problems in the lungs, problems with blood flow, or a problem with the mechanics of breathing. The normal results from CT angiography and other imaging of the lungs suggest that her dyspnea is due to weakness in the muscles of respiration.
What type of muscle tissue is found in the muscles of
respiration?
When specifically questioned about double vision, she reported
that she had had double vision intermittently for the previous
two weeks, which had made it difficult for her to focus on
objects...Her neurological exam revealed mild fatigable ptosis
of the left eye...
Note that in addition to weakness, difficulty eating, and dyspnea, the patient also reports intermittent double vision, which is an uncommon symptom. This combination of symptoms suggests a neuromuscular disorder.
The creatine kinase level was 47 U per liter (reference range, 25-190).
What would cause an elevated level of creatine kinase?
What does the normal creatine kinase level tell you?
In addition to double vision, the neurological exam revealed ptosis, which is drooping of the eyelid. Ptosis and double vision are symptoms that almost always occur in the disorder myasthenia gravis. Myasthenia gravis is an autoimmune disorder in which antibodies to proteins in the neuromuscular junction lead to compromised neuromuscular synaptic transmission and weakness of skeletal muscles.
Testing for acetylcholine-receptor binding, blocking, and modulating antibodies to assess for myasthenia gravis was negative.
The majority of patients with myasthenia gravis have antibodies to the muscle-specific nicotinic acetylcholine receptor. However, a negative test does not rule out the diagnosis of myasthenia gravis, since tests for acetylcholine receptor antibodies are negative in 20% of patients.
Repetitive nerve stimulation with low frequency stimulation to
assess compound muscle action potential amplitude showed
a decrement of more than 10% from normal baseline amplitude in
two nerves.
The repetitive nerve stimulation test is a key test for diagnosis of myasthenia gravis. What is done is a nerve is repetitively stimulated at low frequency (3 stimuli per second), while an electrical recording is made from the muscle that is innervated by that nerve.
What is the term for a recording of muscle electrical activity?
The "compound muscle action potential" ("compound action
potential" in the figure below) is the signal that is
recorded. It is due to the summed action potentials of all
the skeletal muscle fibers in the motor unit.
What electrical signal in the muscle cell is the direct result of acetycholine binding to its receptor?
The neuromuscular junction differs from synapses in the central nervous system in two key ways.
The figure below shows how the response to repetitive nerve
stimulation differs between the normal case (on the left) and in a
patient with myasthenia gravis. Repetitive stimulation of
the nerve depletes acetylcholine in the presynaptic terminal,
causing a decrease in the size of the EPSP. Under normal
circumstances, even when the muscle EPSP decreases due to
repetitive stimulation, it is still well above threshold for
eliciting an action potential. Therefore, there is no change
in amplitude of the compound action potential because every muscle
fiber in the motor unit is still firing an action potential.
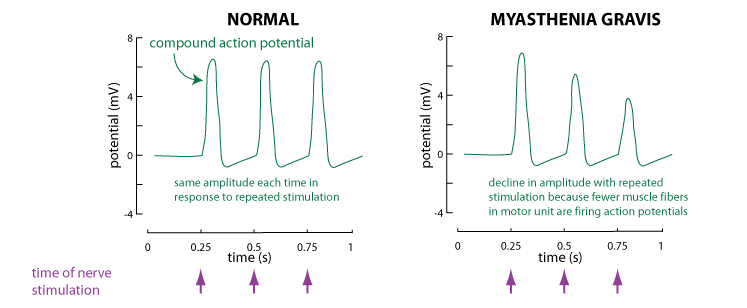
What happens in myasthenia gravis is that there are many fewer
functional acetylcholine receptors at the neuromuscular junction.
So the decrease in acetylcholine release caused by repetitive
stimulation is enough to cause some of the EPSPs to fall below
threshold. If the EPSP is below threshold, the muscle fiber
doesn't fire an action potential. One sees a decline in the
amplitude of the compound action potential because fewer muscle
fibers in the motor unit are firing action potentials.
A diagnosis of myasthenia gravis was made on the basis of the clinical presentation and abnormal results on repetitive nerve stimulation tests...Because the patient's weakness involved swallowing and respiratory muscles, urgent and aggressive therapy was indicated to prevent further deterioration of her condition.
The patient was treated with intravenous immunoglobulin, which
consists of the pooled antibodies from thousands of donors.
Through various mechanisms, intravenous immunoglobulin is capable
of immunosuppression, and so is a powerful tool in the treatment
of autoimmune diseases such as myasthenia gravis.
Additionally, the drug pyridostigmine was prescribed for the patient.
Pyridostigmine is an enzyme inhibitor that is often used in the treatment of myasthenia gravis. What enzyme does pyridostigmine inhibit?
Subsequent antibody testing showed that the patient had
antibodies to muscle-specific kinase, a signaling protein that
plays a role in causing aggregation of acetylcholine receptor
proteins in the motor endplate on the muscle fiber.
Following discharge from the hospital, the patient was treated
with weekly infusions of rituximab, an immunosuppressive drug that
targets antibody-producing cells. At a follow-up visit, her
breathing had improved and her weakness had diminished.