Surgical therapy for obesity is known as bariatric
surgery, from the Greek baros- (meaning
"weight") and iatreia (meaning "medical intervention").
The two most popular surgical approaches used in the United States
are sleeve gastrectomy and Roux-en-Y gastric bypass (RYGB). Both of these procedures
are often performed laparascopically, a minimally invasive
surgical technique in which a small abdominal incision is made and
the surgeon is guided by a laparoscope—a video camera used to
visualize structures in the abdominal cavity.
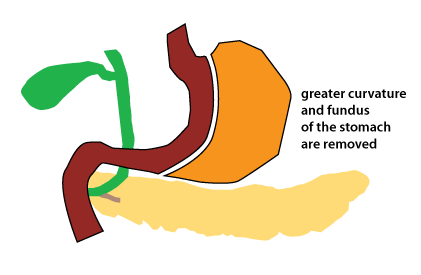
Sleeve gastrectomy involves removing the fundus and the greater curvature of the stomach, so that the stomach becomes a narrow tube (see the figure at right). Initially sleeve gastrectomy was performed as the first stage in a more involved procedure to treat extreme obesity. However, it began being performed as a stand-alone surgery when it was found to cause significant weight loss by itself. It is now the most common bariatric procedure performed.
After sleeve gastrectomy surgery, food intake decreases,
resulting in weight loss. Sleeve gastrectomy greatly reduces
the volume of the stomach, and this may cause earlier satiety (the sense of feeling
"full"), so that the individual eats less. However, the
modern view is that there are a large number of neural and
endocrine changes that probably contribute to weight loss
following sleeve gastrectomy (see below).
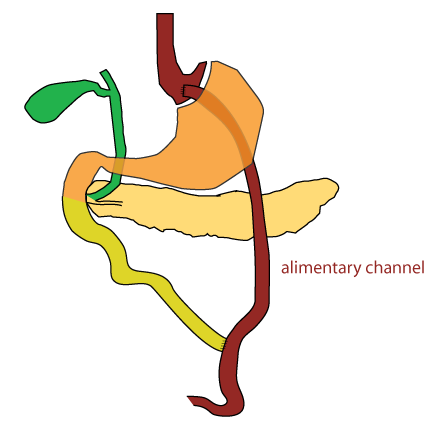
In RYGB, there is a rearrangement of the digestive tract (see
figure at right). The stomach is divided so that a small gastric
pouch is created just below the entry of the esophagus into the
stomach. This is linked to a piece of the lower intestine, usually
the jejunum. This creates an alimentary
channel that bypasses the greater part of
the stomach and the duodenum. The segment consisting of the
stomach and the upper small intestine is linked to the alimentary
channel at a lower point along the small intestine. Important
secretions from the liver (bile) and the pancreas (digestive
enzymes) are still able to enter the GI tract via
this biliopancreatic channel.
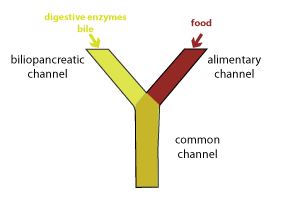
This configuration basically creates a Y. One branch of the Y is the alimentary channel containing food. The other branch of the Y is the upper small intestine containing the biliopancreatic secretions (biliopancreatic channel). Note that digestion and absorption cannot occur until these contents are mixed in the common channel (the stem of the Y).
Since the common channel is shorter than the small intestine
before surgery, RYGB has the potential to cause weight loss by
reducing absorption of nutrients, as well as limiting intake due
to the small size of the stomach pouch. The mechanism of
weight loss does not seem to be related to malabsorption.
Similar to patients who have undergone sleeve gastrectomy,
patients who have had RYGB surgery eat less. Complex
endocrine and neural changes may underlie the reduced food intake
and altered metabolism that promote weight loss.
Because of the bypass of the stomach and duodenum, RYGB creates a situation that can cause the malabsorption of micronutrients (vitamins and minerals). Post-surgery, patients should take vitamin and mineral supplements to avoid micronutrient deficiencies. A common micronutrient deficiency that occurs in people who have had RYGB surgery is iron deficiency.
Both types of bariatric surgery, in addition to producing profound weight loss, are effective in causing remission of type 2 diabetes mellitus (T2DM). T2DM is a disorder that is characterized by hyperglycemia (high blood glucose) and insulin resistance, which is a decreased sensitivity to insulin. Patients with T2DM also usually have defects in insulin secretion. The majority of people with T2DM are overweight or obese.
Remission means a reduction in blood glucose to normal levels without the need for diabetes medication. Profound weight loss probably plays a role in improving insulin sensitivity. However, many patients with T2DM begin to show improvements in insulin sensitivity within the first few weeks after surgery, well before they lose weight. This is particularly true for patients who have undergone RYGB. It is thought that the rearrangement of the digestive tract somehow causes endocrine changes that are beneficial.
Effects on three key hormones are thought to play a major role in
weight loss and remission of T2DM that occurs in patients who have
had bariatric surgery.
The regulation of satiety and nutrient homeostasis is complicated and other factors are likely to be involved.
Two randomized trials published in January 2018 comparing sleeve gastrectomy with RYGB found little difference in the weight loss achieved after five years. There were also similar rates for remission of type 2 diabetes mellitus between the two types of surgery, although the numbers were better for RYGB. One notable difference is that in patients with gastroesophageal reflux disease (GERD) there tended to be improvement following RYGB; however, GERD was found to worsen or newly arise in some patients following sleeve gastrectomy.
A larger trial published in 2020 that focused on diabetes mellitus outcomes found that RYGB was slightly better than sleeve gastrectomy for achieving remission of T2DM.
If you are interested, there are links to the articles reporting
on these studies in the darker blue "Optional" section below the
quick quiz.
For a review discussing how bariatric surgery causes remission
of T2DM, see: Abbasi, J.(2017) Unveiling the "Magic" of Diabetes
Remission After Weight-Loss Surgery JAMA 317(6):
571-4 (link)
Here are the references to the two studies that compared sleeve gastrectomy and RYGB: