Celiac disease (also known as gluten enteropathy or celiac sprue) is a disorder of malabsorption that occurs when there is an inappropriate immune response to gluten, a protein found in wheat. Celiac disease was once thought to be a fairly rare disorder of children, but it is now recognized that celiac disease can develop in adulthood, that there can be a range of disease severity, and that the disorder may be fairly common (perhaps affecting as many as 1 in 100 people in certain parts of Europe and North America).
Celiac disease is NOT an allergy to wheat. The term allergy, although imprecise, is usually used to describe immediate hypersensitivity disorders that involve the generation of IgE antibodies (for instance hay fever is an allergy to pollen). When exposed to an allergen, the response is within minutes. By contrast, celiac disease is a type of autoimmune disease. The immune response is a delayed response (on the course of hours to days) and involves helper T cells, which coordinate an immune response leading to tissue damage in the small intestine (see below).
There is a genetic component to celiac disease. All individuals who develop celiac disease express particular alleles of one type of MHC molecule. Other genetic and environmental factors probably play a role in the expression of the disease, since many more people carry these particular MHC alleles than have celiac disease, and many people don't develop celiac disease until late adulthood.
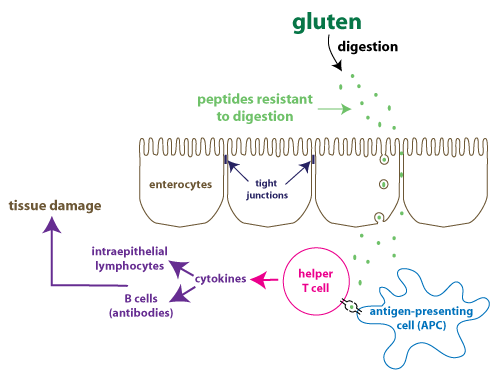
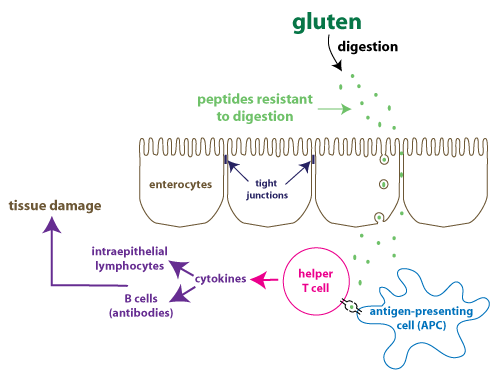
The figure shows a simplified illustration of our understanding of the pathogenesis of celiac disease. Peptides derived from gluten contain many proline and glutamine residues, making them resistant to digestion by pancreatic and small intestine enzymes. These peptides gain access to the lamina propria, the connective tissue layer immediately underlying the epithelium where gut-associated lymphoid tissue (GALT) is located. GALT is the immune tissue that is found along the GI tract. Gluten-derived peptides cross the intestinal epithelium either by transcytosis or by a paracellular route (moving between cells). Paracellular transport would involve a breakdown in the tight junctions between enterocytes to cause an increase in intestinal permeability. There is some evidence that increased intestinal permeability occurs more frequently in individuals with celiac disease.
Once in the lamina propria, an enzyme modifies these peptides,
making them even more antigenic. They are engulfed by antigen presenting cells (APC's) which display them on their
surface bound to MHC II molecules.
They stimulate helper T cells,
which secrete cytokines that
orchestrate the inflammatory response that leads to tissue
damage. One cytokine in particular (IL-15) stimulates intraepithelial
lymphocytes. Intraepithelial lymphocytes
are related to cytotoxic T cells and are specifically found in
mucosal linings such as the GI tract. IL-15 promotes their
proliferation, survival, and cell-killing properties.
The consequence of the tissue damage is a change in the mucosa in the small intestine.
This can be observed in a duodenal
biopsy, which is a key test in the diagnosis of
celiac disease. Instead of the normal architecture of tall villi and deep crypts, what is observed in celiac
disease is a flattened mucosa
lacking villi. This can greatly decrease the surface area of the
small intestine, causing malabsorption of nutrients, which can
cause diarrhea and malnutrition. Duodenal tissue also shows
increased numbers of intraepithelial
lymphocytes. In class we will look at
histology images showing flattened mucosa.
There is a broad range in the severity of symptoms. When the
disease is detected in early childhood, it usually causes severe
malabsorption, diarrhea, and a failure to thrive. Adults with
celiac disease may have diarrhea and experience weight loss, but
often the initial clinical presentation is iron-deficiency
anemia. This occurs because the mucosal changes are
concentrated in the duodenum,
where iron absorption takes place. Some individuals with an immune
response to gluten do not have gastrointestinal symptoms at all,
but instead get a skin rash, which is termed dermatitis herpetiformis.
Antibodies that are produced in the immune response to gluten
cross-react with a skin antigen to trigger dermatitis
herpetiformis. In some rare cases, celiac disease may even
cause neurological symptoms.
At present, the only treatment for celiac disease is a totally gluten-free diet. This is not as
easy as it sounds, since gluten is a frequent additive to many
prepared foods, or may be a contaminant of foods such as oats.
A promising treatment approach is the development of a glutenase,
an enzyme that would be capable of digesting the immunostimulatory
peptides to prevent the autoimmune response. Ideally, the
enzyme would be able to work in the acidic environment of the
stomach so that the peptides would be destroyed before they
reached the duodenum. Such a treatment would be useful in
people with refractory celiac disease. These are individuals
who continue to experience symptoms even when they adhere to a
gluten-free diet. Furthermore, an effective glutenase would
mean that people with celiac disease could be less vigilant about
keeping all gluten out of their diet. Work that began with
undergraduate researchers at the UW has led to the development of
a promising glutenase therapy (see the Optional box below).
In 2011, a team of UW undergraduates won top prize in an international synthetic biology engineering competition for their work in engineering an enzyme that could digest gliadin at the low pH of the stomach. (Gliadin is the proline and glutamine-rich polypeptide in gluten that resists digestion and causes the immune response). This link describes their prize-winning project.
This work has also been published in: Gordon, S.R. et al.
(2012) Computational Design of an Alpha-Gliadin Peptidase. J.
Am.
Chem. Soc. 134(50): 20513-20520 (link)
In September of 2018, PvP Biologics began a phase 1 clinical trial to test their engineered enzyme in human subjects. After successful completion of the phase 1 clinical trial, PvP Biologics was acquired by Takeda Pharmaceuticals for $330 million in February 2020:link
The results of the phase 1 trial of the engineered enzyme (now
called TAK-062) have been published: Pultz, I.S. et al.Gluten
Degradation, Pharmacokinetics, Safety, and Tolerability of
TAK-062, an Engineered Enzyme to Treat Celiac Disease (2021) . Gastroenterology
161(1): 81-93 (link)