Atherosclerosis is a
cardiovascular disease in which plaques
form in the tunica intima of blood
vessels. Atherosclerosis is an inflammatory
disease, and tends to develop in sites where the endothelium becomes
damaged. Useful reading in the Silverthorn textbook is
found on pages 501-504, particularly Figure 15.21 (p.
503), which describes the development of atherosclerotic
plaque.
Heart disease occurs because the coronary
arteries supplying the heart are a major site where
atherosclerotic plaques form. The growth of atherosclerotic
plaque can cause blood vessels to narrow, reducing blood flow, and
causing chest pain (angina).
Even more damaging is when a plaque ruptures and triggers the
formation of a clot, which blocks blood flow and oxygen delivery
causing tissue damage. When a clot blocks blood flow in a
coronary artery, this is known as a myocardial
infarction (heart attack).
The major factors that increase the risk for atherosclerotic
cardiovascular disease are male sex, increased age, smoking, high
blood pressure, and dyslipidemia.
Dyslipemia means abnormal levels of circulating lipids.
Increased risk for atherosclerotic cardiovascular disease is
associated with a high level of LDL
cholesterol and a low
level of HDL cholesterol. But what do we mean
when we say "LDL cholesterol"?
Cholesterol is a lipid that
is an important component of cell membranes and is the precursor
used in the synthesis of steroid hormones, bile salts (necessary
for fat digestion and absorption), and vitamin D.
Cholesterol, like other lipids, is nonpolar and poorly soluble in
the aqueous extracellular fluid. Cholesterol and other
lipids travel through the circulation packaged in particles called
lipoproteins.
Lipoproteins are particles that contain several thousand
molecules. The core of the lipoprotein is filled with
nonpolar molecules: cholesterol
esters and triacylglycerol
(TAG; fat). The outer layer of the lipoprotein is coated
with amphipathic phospholipids
in a single layer, oriented so that their nonpolar tails face the
core of the lipoprotein and their polar heads face outward,
enabling the lipoprotein to be soluble in the fluids of the
body. The outside of the lipoprotein contains amphipathic
proteins called apolipoproteins
that stabilize the lipoprotein and provide an identity tag.
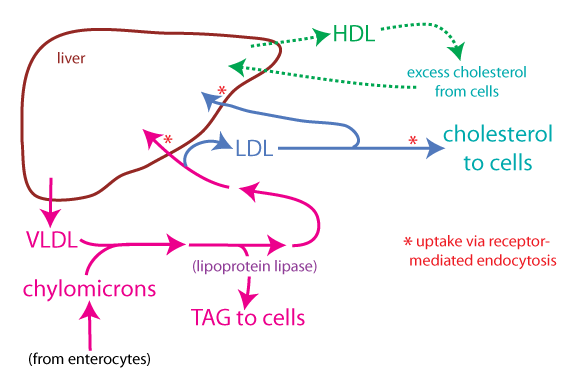
Lipoproteins can be differentiated on the basis of their density, but also by the types of apolipoproteins they contain. The degree of lipid in a lipoprotein affects its density—the lower the density of a lipoprotein, the more lipid it contains relative to protein. The four major types of lipoproteins are chylomicrons, very low-density lipoprotein (VLDL), low-density lipoprotein (LDL), and high-density lipoprotein (HDL).
Although all cells can make cholesterol, cholesterol is mainly
synthesized in the liver by hepatocytes.
Hepatocytes also synthesize triacylglycerol (TAG) from excess
carbohydrates. Hepatocytes package cholesterol and TAG in
lipoproteins for export to other cells in the body.
The figure below summarizes the fates of the various lipoproteins. Refer to it as you read about the different lipoproteins.
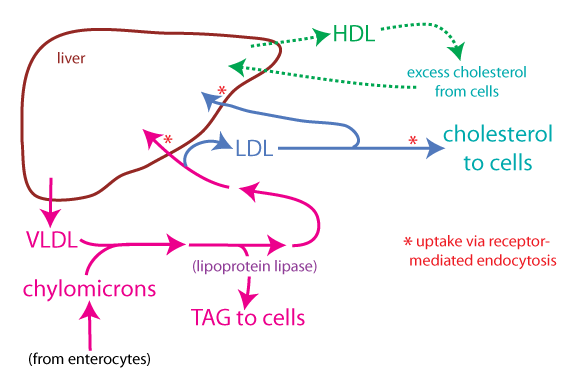
The liver is central to the regulation of cholesterol levels in the body. Not only does it synthesize cholesterol for export to other cells, but it also removes cholesterol from the body by converting it to bile salts and putting it into the bile where it can be eliminated in the feces. Furthermore, the liver synthesizes the various lipoproteins involved in transporting cholesterol and other lipids throughout the body.
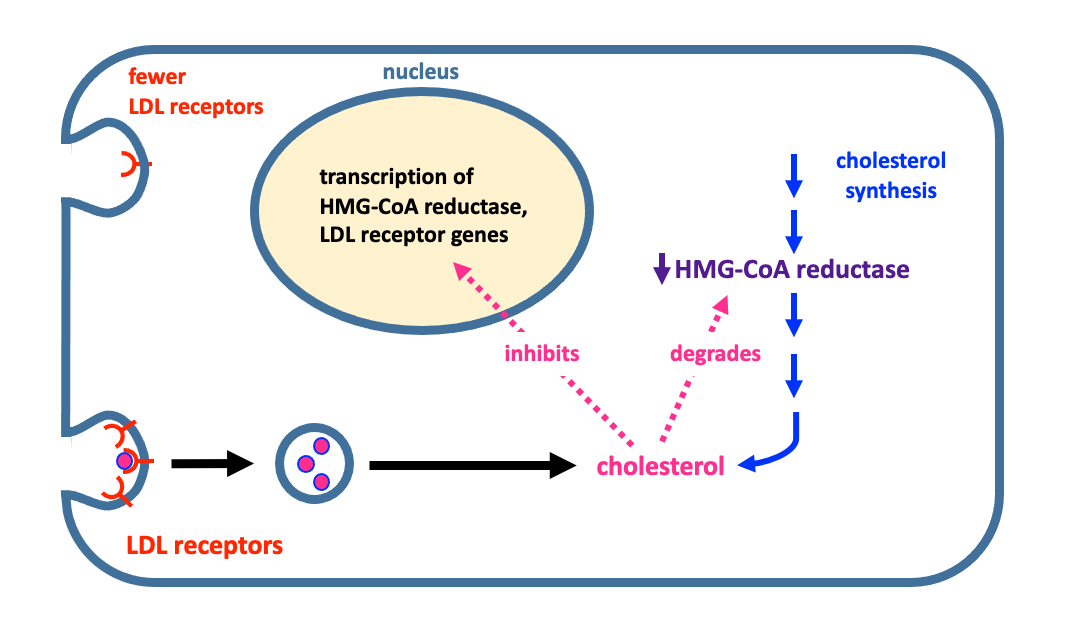 Cholesterol synthesis in the liver is under negative feedback regulation.
The rate-limiting step in cholesterol synthesis involves the
enzyme HMG-CoA reductase.
Increased cholesterol inside the hepatocyte causes decreased
HMG-CoA reductase activity by causing degradation of the
enzyme. Cholesterol also inhibits a factor that travels to
the nucleus to stimulate trasncription of LDL receptors and
HMG-CoA reductase. As shown in the figure, when cholesterol
is high inside the hepatocyte, it has two responses that can lower
cholesterol:
Cholesterol synthesis in the liver is under negative feedback regulation.
The rate-limiting step in cholesterol synthesis involves the
enzyme HMG-CoA reductase.
Increased cholesterol inside the hepatocyte causes decreased
HMG-CoA reductase activity by causing degradation of the
enzyme. Cholesterol also inhibits a factor that travels to
the nucleus to stimulate trasncription of LDL receptors and
HMG-CoA reductase. As shown in the figure, when cholesterol
is high inside the hepatocyte, it has two responses that can lower
cholesterol:
Conversely, when cholesterol is low inside the hepatocyte, it upregulates cholesterol synthesis through increased transcription of HMG-CoA reductase. And it upregulates cholesterol clearance from the circulation by increasing expression of LDL receptors. The LDL receptor is key to the regulation of cholesterol levels in the body, because it allows the hepatocyte to "see" how much LDL is in the circulation.
The link between cholesterol and heart disease was recognized
through the study of individuals with familial
hypercholesterolemia (FH).
There are two forms of FH: a severe homozygous form which is
very rare (affecting 1 in 1,000,000 individuals) and a more common
heterozygous form (affecting 1 in 500 individuals).
Individuals with heterozygous FH have levels of LDL that are
roughly twice as high as normal, and they may start to have heart
attacks and strokes in their 30s and 40s. In the more severe
homozygous form of FH, LDL is 3-6 times higher than normal and
heart attacks and strokes occur in childhood. FH clearly
illustrates that there is a link between the level of LDL
cholesterol and the risk for atherosclerotic cardiovascular
disease.
The genetic defect in FH was determined through the work of
Michael Brown and Joseph Goldstein (for which they were awarded
the 1985 Nobel Prize in Physiology or Medicine). Most FH is caused by a mutation in the LDL
receptor. In FH homozygotes without
functioning LDL receptors, LDL is not cleared from the
circulation. As well, because cholesterol cannot get into cells
efficiently, there is no negative feedback suppression of
cholesterol synthesis in the liver.
Another mutation that can cause FH is a mutation in apolipoprotein B, the
apolipoprotein found in LDL. Apolipoprotein B is the
component of LDL that specifically binds to the LDL receptor.
More common in the general population is dyslipidemia, which is the term that is used if lipid levels are outside the normal range. In a typical lipid profile, the fasting levels of total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides are determined. High levels of LDL cholesterol (the so-called “bad cholesterol”) greatly increase the risk for atherosclerosis because LDL particles contribute to the formation of atherosclerotic plaques. Low levels of HDL cholesterol (the so-called "good cholesterol") are an independent risk factor, because reverse cholesterol transport works to prevent plaque formation, or may even cause regression of plaques once they have formed. HDL may also have anti-inflammatory properties that help reduce the risk of atherosclerosis. Fasting triglyceride levels are used to estimate the level of VLDL. High levels of triglycerides are also associated with an increased risk for atherosclerosis, although the mechanism is not entirely clear.
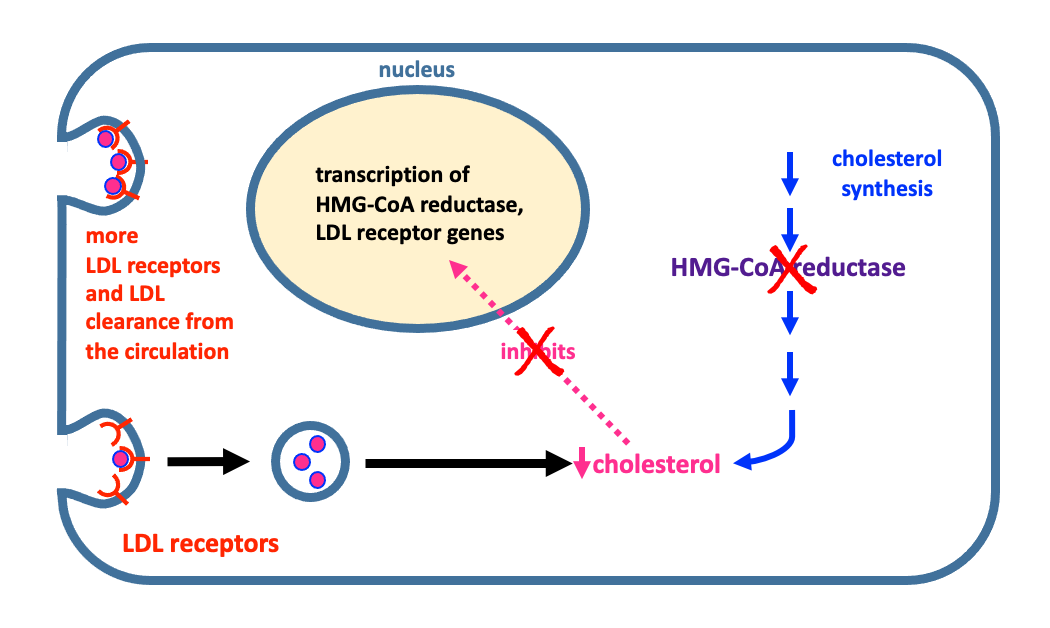 The
most important drugs for the treatment of dyslipidemia are by far,
the statins. Statins have been shown in multiple clinical trials
to reduce cardiovascular events and mortality.
The
most important drugs for the treatment of dyslipidemia are by far,
the statins. Statins have been shown in multiple clinical trials
to reduce cardiovascular events and mortality.
In the past, several different drugs have been used to treat dyslipidemia, however the most recent treatment guidelines recommend mainly statin therapy at different intensities according to the patient's risk for cardiovascular disease. However, statins may cause adverse effects in some patients, or in others, statins by themselves may not provide sufficient lowering of LDL cholesterol. These patients may benefit from the use of the other two drugs listed below.
Two PCSK9 inhibitor drugs were approved in 2015: alirocumab (Praluent™) and evolocumab (Repatha™). Because they are monoclonal antibody drugs, they must be administered by injection. In December 2021, the FDA approved inclisiran (Leqvio™) a small interfering RNA drug that is also a PCSK9 inhibitor.
PCSK9 inhibitors have been approved as a second-line
treatment for patients who can’t tolerate statins, or who are
unable to get effective lowering of LDL cholesterol by using a
statin alone. In clinical trials, these drugs were able to
substantially lower LDL cholesterol. Large randomized,
controlled clinical trials have shown that treatment with
PCSK9 inhibitors can lower cardiovascular events such as heart
attack and stroke. Because of their high cost and the
requirement that they be administered by injections, PCSK9
inhibitors are mainly recommended for use in high risk
patients, such as patients with familial hypercholesterolemia.
*PCSK9 stands for "proprotein convertase subtilisin/kexin type 9".