Hormonal Contraception
Mechanism of Action
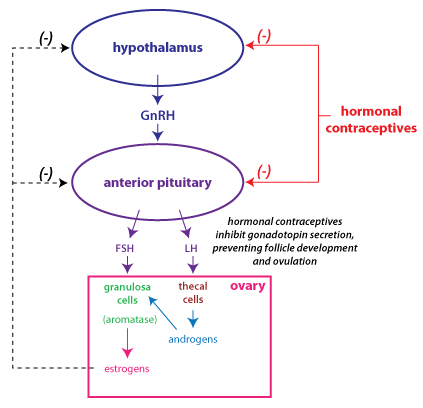 The primary mechanism of action of hormonal
contraceptives is that they suppress the secretion of gonadotropins (follicle stimulating hormone, FSH and luteinizing
hormone, LH)
by mimicking feedback inhibition (shown
in
the figure at right). Through various means of delivery (oral,
depot injection, implant, transdermal), a woman receives a
combination of estrogen and progesterone, or just progesterone by
itself. Progesterone with estrogen naturally inhibits gonadotropin
secretion as, for instance, during the luteal phase of the cycle.
The goal is to suppress ovulation.
The inhibition provided by hormonal contraceptives prevents the
rise in FSH that is necessary to initiate the growth phase of
follicle development and selection of a dominant follicle. This
inhibition also prevents the LH surge that is necessary to trigger
ovulation.
The primary mechanism of action of hormonal
contraceptives is that they suppress the secretion of gonadotropins (follicle stimulating hormone, FSH and luteinizing
hormone, LH)
by mimicking feedback inhibition (shown
in
the figure at right). Through various means of delivery (oral,
depot injection, implant, transdermal), a woman receives a
combination of estrogen and progesterone, or just progesterone by
itself. Progesterone with estrogen naturally inhibits gonadotropin
secretion as, for instance, during the luteal phase of the cycle.
The goal is to suppress ovulation.
The inhibition provided by hormonal contraceptives prevents the
rise in FSH that is necessary to initiate the growth phase of
follicle development and selection of a dominant follicle. This
inhibition also prevents the LH surge that is necessary to trigger
ovulation.
There are other ways that hormonal contraceptives interfere with
conception. One important strategy is to interfere with the
movement of sperm in the female reproductive tract. Sperm are
deposited in the vagina and must traverse the cervix. In the follicular phase,
estrogen promotes the production of thin, watery
mucus by the cervical glands. By contrast, progesterone promotes
secretion of thick cervical mucus,
which acts as a barrier, and inhibits
sperm movement past the cervix. This effect
on the cervical mucus is particularly important for the efficacy
of low-dose progesterone-only oral contraceptives, because the low
dose of progesterone may not consistently suppress ovulation.
Types
Combination contraceptives
Combination contraceptives contain both an estrogen and a
progestin (a drug that binds to progesterone receptors). In
typical formulations, a pill is taken every day for three weeks,
with one week of placebo pills. During the week when she is
taking the placebo pills, the woman experiences a withdrawal
bleed. The withdrawal bleed serves as a convenient signal
that the woman has not become pregnant, but it is not essential.
There are also continuous-use oral contraceptives that eliminate
the placebo pills. Continuous-use contraceptive pills are
designed for women who would like to have fewer menstrual periods
because they suffer from menorrhagia (excessive
menstrual bleeding) or dysmenorrhea (painful
menstruation).
Because steroid hormones are nonpolar, they can be
delivered topically. Combination contraceptives using this method
of administration are a patch that is changed weekly, and a
vaginal ring that is inserted and left in place for three weeks.
Progesterone-only contraceptives
There are several different types of contraceptives that use only
progestins. The long-acting methods are useful in those women who
don’t want to or can’t remember to take a pill every day. Another
advantage to these methods is that the woman may have medical
reasons to avoid exposure to increased levels of estrogen.
Low-dose pills
These are not as effective as combination contraceptives at
preventing ovulation. Their effectiveness depends upon the ability
of progesterone to alter the cervical mucus. It is very important
for these pills to be taken at the same time each day, so that the
plasma level of the progestin is sufficient to affect the cervical
mucus.
Why would a woman opt for this method if it is less effective?
This type of contraceptive is useful in women who need to avoid
estrogen. Also, low-dose progesterone only contraceptives
are recommended for use in women who are lactating and don’t wish
to become pregnant because high levels of estrogen and
progesterone inhibit milk synthesis.
Long-acting methods
Long-acting progesterone-only
contraceptives are the most effective methods of hormonal
contraception. These methods include an
implantable rod that releases a progestin (Nexplanon®),
an intrauterine device (IUD) that releases a progestin, and an
injection (Depo-Provera®) that is given once every 3
months. The progestin diffuses out at a steady rate to
prevent ovulation through negative feedback inhibition, and to
prevent fertilization through changes to the cervical mucus.
Of these methods, the implantable rods and the IUD have greater
contraceptive efficacy because once they are inserted they work
effectively for several years without any other action
required. By contrast, the Depo-Provera shot requires that
the woman get a shot every 3 months, and delays in getting the
shot decrease contraceptive efficacy.
A concern with the injection method, Depo-Provera, has been that
it causes enough inhibition of estrogen production by the ovary to
cause a decrease in bone density. (Estrogen maintains bone
density by preventing bone resorption through inhibition of
osteoclasts.) However, the decrease in bone density is small, and
appears to reverse after contraceptive use is discontinued.
Emergency contraception
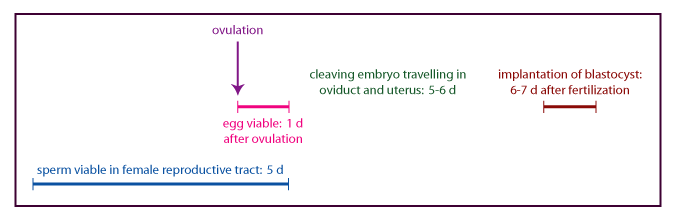
Emergency contraception is hormonal contraception that is used by
a woman after she has had unprotected intercourse. Note the timing
of events surrounding fertilization as depicted in the figure
below. Because sperm are viable for several days, and because
women can’t be sure of the exact timing of ovulation, it may be
possible to prevent fertilization by a contraceptive method that
blocks or delays ovulation.
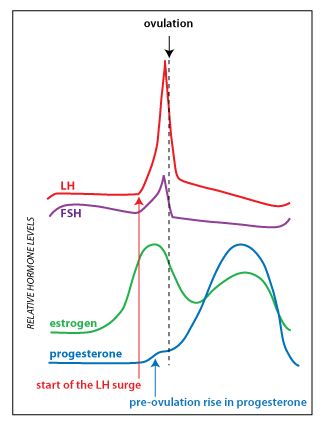
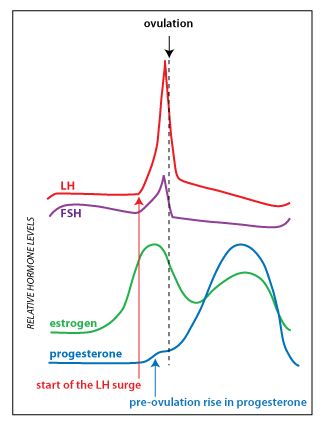 The
emergency
contraceptive pill Plan B® uses a higher dose of progestin (levonorgestrel) than found in
typical oral contraceptives. It works by delaying or inhibiting
ovulation via the same mechanism (feedback inhibition of
gonadotropin secretion) as conventional hormonal contraception. In
a study in which LH levels were measured (as a marker for
ovulation), it was found that levonorgestrel emergency
contraception only worked when taken before the LH
surge. The figure at right shows the pattern of hormone secretion
and indicates the start of the LH surge (red arrow). Plan B
is most effective when used within 12 hours of
unprotected intercourse, but can be effective for up to 5 days
(120 hours) following unprotected intercourse.
The
emergency
contraceptive pill Plan B® uses a higher dose of progestin (levonorgestrel) than found in
typical oral contraceptives. It works by delaying or inhibiting
ovulation via the same mechanism (feedback inhibition of
gonadotropin secretion) as conventional hormonal contraception. In
a study in which LH levels were measured (as a marker for
ovulation), it was found that levonorgestrel emergency
contraception only worked when taken before the LH
surge. The figure at right shows the pattern of hormone secretion
and indicates the start of the LH surge (red arrow). Plan B
is most effective when used within 12 hours of
unprotected intercourse, but can be effective for up to 5 days
(120 hours) following unprotected intercourse.
Another oral emergency contraceptive pill, ulipristal
(marketed as ella®) was approved in 2010. Ulipristal is
classified as a selective progesterone
receptor modulator. In the ovary, it acts as a progesterone antagonist that
blocks progesterone action in the follicle. Note that there is a
small increase in progesterone secretion induced by the LH surge,
and it appears that this is necessary for ovulation to occur (blue
arrow in figure). An advantage of ulipristal is that it is still
effective at delaying ovulation even if it taken after the
beginning of the LH surge. Ulipristal is not effective if
taken after the peak of the LH surge.
Progesterone is necessary to maintain the endometrium for
implantation. Thus, it is theoretically possible that ulipristal
may work to prevent pregnancy through post-fertilization
mechanisms. However, ulipristal used for emergency
contraception is at a low dose that is not likely to affect the
endometrium. A study from 2019 concluded that ulipristal is
unlikely to have any effect on implantation.
Risks
Many women use hormonal contraceptives without experiencing any
adverse effects, while some experience minor adverse effects such
as abnormal menstrual bleeding, or weight gain. Below, only the
most serious adverse effects of hormonal contraceptives are
considered, followed by a discussion of the various benefits of
hormonal contraceptives.
Cardiovascular risks
Cardiovascular disorders comprise the most serious adverse
effects associated with hormonal contraceptives. Although oral
contraceptives increase the risk for certain cardiovascular
disorders, these disorders are extremely rare among young women. A
key thing to keep in mind is that pregnancy increases
the risk for these cardiovascular disorders to a greater
degree than hormonal contraceptives.
Hormonal contraceptives promote
thrombosis (the formation of a blood clot).
The synthetic hormones in hormonal contraceptives have a variety
of effects on the coagulation system that make the formation of a
clot more likely. Clot formation in the venous system is known as
venous thromboembolism (VTE), the most serious consequence
being a pulmonary embolism. If a clot forms in the
arterial system, it can lead to a myocardial infarction or
stroke. The increase in clotting is thought to be
primarily an effect of estrogen.
Hormonal contraceptives increase the risk for venous
thromboembolism. This increased risk was higher with the earliest
formulations of contraceptives that used higher doses of estrogen.
Current formulations of oral combination contraceptives increase
the risk of VTE from 3-6 fold. This seems high, but it is
important to note that the absolute risk of VTE among
young, reproductive age women is only 1 in 10,000. Oral
contraceptive use also increases the risk of myocardial infarction
and stroke, particularly among older users who smoke.
Breast cancer
Because many breast tumors may have their growth stimulated by
estrogen, it is reasonable to think that estrogen-containing
contraceptives might increase the risk of breast cancer. Several
large case-control studies have shown there is no increase
in the risk of breast cancer among current and former users of
combined contraceptives, however these studies focused on older
women. There is evidence of an increased risk of breast cancer
among young hormonal contraceptive users compared to young
non-users. It is important to keep in mind that the number of
young women who get breast cancer is very, very low—most breast
cancers are diagnosed in post-menopausal women.
Benefits
The major benefit of hormonal contraceptives is reliable,
reversible contraception. Hormonal contraceptives are the most
effective methods of reversible contraception available to woman,
being 97-99% effective if used properly. Furthermore, there are a
number of non-contraceptive benefits associated with hormonal
contraceptives.
Menstrual symptoms
Because hormonal contraceptives decrease endometrial
proliferation, they are beneficial for women who suffer from menorrhagia
or dysmenorrhea. They are particularly helpful for
treating women with polycystic ovary
syndrome who do not wish to conceive, because they
reduce endometrial proliferation
and normalize menstrual periods.
Endometrial cancer
Decreased endometrial proliferation probably also underlies the
positive effect on rates of endometrial
cancer. Hormonal contraceptive use decreases the
risk of endometrial cancer, with longer duration of use causing a
greater protective effect.
Ovarian cancer
Many studies have shown a decreased risk for the development of
ovarian cancer among women who have ever used hormonal
contraceptives. Like endometrial cancer, the reduction in risk is
greatest for those women who have used hormonal contraception the
longest. The hypothesis is that reduced risk is related to
reducing the lifetime number of ovulations, since there is also a
reduction in ovarian cancer risk associated with having been
pregnant.
Androgen secretion
Hormonal contraceptives are used to treat hyperandrogenism
because they decrease gonadotropin stimulation of androgen
production by the ovary. Androgens may cause masculinization, and
they also stimulate the production of sebum, which promotes acne.
Randomized, placebo-controlled trials have shown that oral
contraceptives are better than placebo at reducing the severity of
acne.
Further Reading (optional)
Optional
For those that are further interested in this topic, here are
some useful review articles.
- Marchbanks, P. A. et al. (2002) Oral Contraceptives and the
Risk of Breast Cancer. New England Journal of Medicine
346: 2025-32 (link)
- Petitti, D. B. (2003) Combination Estrogen-Progestin Oral
Contraceptives. New England Journal of Medicine 349:
1443-50 (link)
- Kaunitz, A. M. (2008) Hormonal Contraception in Women of
Older Reproductive Age. New England Journal of Medicine
358: 1262-70 (link)
- Gemzell-Danielsson, K. (2010) Mechanism of Action of
Emergency Contraception. Contraception 82(5): 404-409
(link)
- Raymond, E. G. and Cleland, K. (2015) Emergency
Contraception. New England Journal of Medicine 372:
1342-8 (link)
- Curtis, K. M. and Peipert, J. F. (2017) Long-Acting
Reversible Contraception. New England Journal of Medicine
376: 461-8 (link)
- Hunter, D.J. (2017) Oral Contraceptives and the Small
Increase of Breast Cancer. New England Journal of Medicine
377: 2276-7 (link)
- Li, H. W. R. et al. (2019) Does ulipristal acetate emergency
contraception (ella®) interfere with implantation?
Contraception 100(5): 386-90 (link)
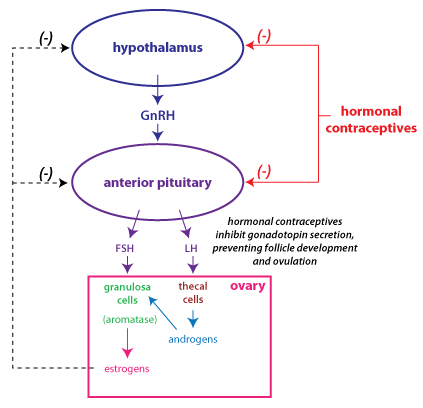 The primary mechanism of action of hormonal
contraceptives is that they suppress the secretion of gonadotropins (follicle stimulating hormone, FSH and luteinizing
hormone, LH)
by mimicking feedback inhibition (shown
in
the figure at right). Through various means of delivery (oral,
depot injection, implant, transdermal), a woman receives a
combination of estrogen and progesterone, or just progesterone by
itself. Progesterone with estrogen naturally inhibits gonadotropin
secretion as, for instance, during the luteal phase of the cycle.
The goal is to suppress ovulation.
The inhibition provided by hormonal contraceptives prevents the
rise in FSH that is necessary to initiate the growth phase of
follicle development and selection of a dominant follicle. This
inhibition also prevents the LH surge that is necessary to trigger
ovulation.
The primary mechanism of action of hormonal
contraceptives is that they suppress the secretion of gonadotropins (follicle stimulating hormone, FSH and luteinizing
hormone, LH)
by mimicking feedback inhibition (shown
in
the figure at right). Through various means of delivery (oral,
depot injection, implant, transdermal), a woman receives a
combination of estrogen and progesterone, or just progesterone by
itself. Progesterone with estrogen naturally inhibits gonadotropin
secretion as, for instance, during the luteal phase of the cycle.
The goal is to suppress ovulation.
The inhibition provided by hormonal contraceptives prevents the
rise in FSH that is necessary to initiate the growth phase of
follicle development and selection of a dominant follicle. This
inhibition also prevents the LH surge that is necessary to trigger
ovulation.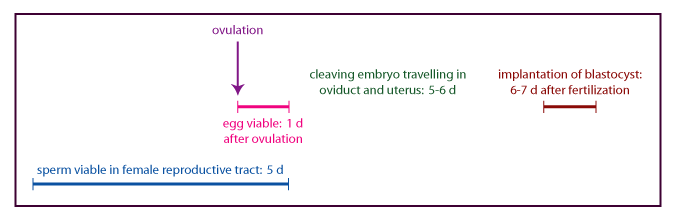
 The
emergency
contraceptive pill Plan B® uses a higher dose of progestin (levonorgestrel) than found in
typical oral contraceptives. It works by delaying or inhibiting
ovulation via the same mechanism (feedback inhibition of
gonadotropin secretion) as conventional hormonal contraception. In
a study in which LH levels were measured (as a marker for
ovulation), it was found that levonorgestrel emergency
contraception only worked when taken before the LH
surge. The figure at right shows the pattern of hormone secretion
and indicates the start of the LH surge (red arrow). Plan B
is most effective when used within 12 hours of
unprotected intercourse, but can be effective for up to 5 days
(120 hours) following unprotected intercourse.
The
emergency
contraceptive pill Plan B® uses a higher dose of progestin (levonorgestrel) than found in
typical oral contraceptives. It works by delaying or inhibiting
ovulation via the same mechanism (feedback inhibition of
gonadotropin secretion) as conventional hormonal contraception. In
a study in which LH levels were measured (as a marker for
ovulation), it was found that levonorgestrel emergency
contraception only worked when taken before the LH
surge. The figure at right shows the pattern of hormone secretion
and indicates the start of the LH surge (red arrow). Plan B
is most effective when used within 12 hours of
unprotected intercourse, but can be effective for up to 5 days
(120 hours) following unprotected intercourse.