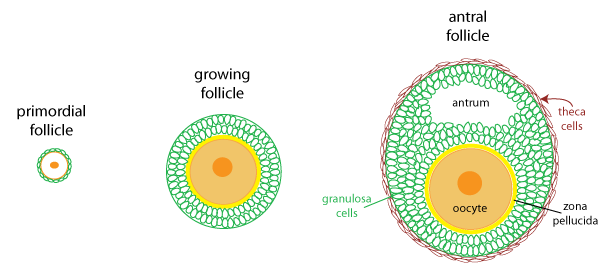
The germ cells (cells that will give rise to gametes) that are present in the ovary are oocytes. Each oocyte develops within a structure of support cells called a follicle. Non-developing follicles are called primordial follicles, and consist of a single layer of undifferentiated follicle cells surrounding an oocyte. When a follicle starts to develop, the follicle cells differentiate to become rounded granulosa cells, which start to proliferate. The oocyte enlarges, and a layer of glycoproteins called the zona pellucida forms between the granulosa cells and oocyte. The enlarging granulosa cell layer is surrounded by a basement membrane. Eventually, larger follicles start to accumulate spindle-shaped thecal cells outside the basement membrane. Within the granulosa cell layer, a fluid-filled space called the antrum develops.
The development of oocytes and ovulation occurs in a monthly
cycle that depends upon hormonal interactions between the
hypothalamus, anterior pituitary, and ovary. The cycle
starts in the ovary with the growth phase, when some
antral follicles begin to develop and enlarge under the influence
of the gonadotropin hormones FSH
(follicle stimulating hormone) and LH
(luteinizing hormone). By the end of the first week,
only a single follicle will be mature enough to continue
developing; this is called the dominant follicle. The rest
of the follicles will degenerate, in a process known as atresia. Atresia is the fate
for all but a few hundred follicles in the ovary.
In the second week of the cycle, the dominant follicle enlarges to become a mature follicle, bulging out on the surface of the ovary and reaching a final size of between 1 and 3 centimeters. Ovulation occurs at the end of the second week when the follicle ruptures to release the egg to the fluid surrounding the ovary.
Following ovulation, the remaining cells of the follicle differentiate into the corpus luteum. The granulosa cells greatly increase in size, the basement membrane breaks down, and the structure is invaded by blood vessels. The corpus luteum is an important endocrine structure, secreting progesterone and estrogen that is necessary to prepare the uterus for implantation and early pregnancy. The corpus luteum persists as long as there is sufficient hormonal support. In a typical menstrual cycle, it degenerates between day 25 and 28 when LH levels decline. If a fertilized embryo implants in the uterus, the hormone chorionic gonadotropin is made. Chorionic gonadotropin is an LH analogue (meaning it binds to LH receptors) that stimulates the corpus luteum to grow and persist throughout the first trimester of pregnancy. Pregnancy tests are an assay for chorionic gonadotropin in the urine.
The pink timeline below the hormone graph summarizes the important ovarian events. Note that ovulation divides the cycle in half: the first half, when follicles develop is the follicular phase, the second half when the corpus luteum is active is the luteal phase.
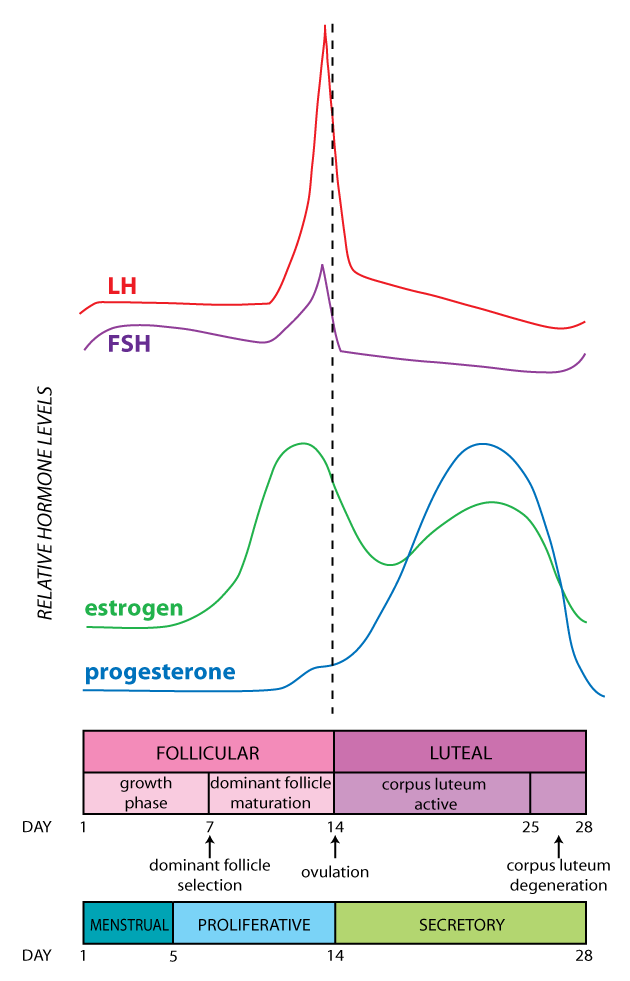
There is an interplay between ovarian events and gonadotropin
secretion from the anterior pituitary that results in a cyclical
pattern of hormone secretion in the female. The graph at right
depicts the relative average daily levels of LH, FSH, estrogen,
and progesterone throughout the cycle. Refer to this figure
as you read through the next section.
The initial growth of follicles at the beginning of the cycle is due to the small increase in FSH and LH that occurs when estrogen and progesterone levels decline at the end of the previous cycle, releasing the hypothalamus and anterior pituitary from feedback inhibition.
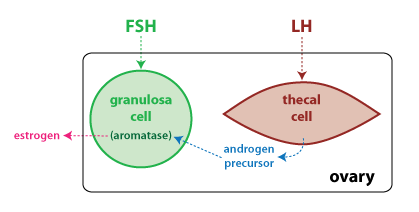
As follicles grow, they start to secrete increasing amounts of estrogen in response to stimulation from gonadotropins. The two cell types collaborate in the production of estrogen (see figure below). Granulosa cells express the enzyme aromatase, which converts an androgen precursor to estrogen; however they lack the enzymes to make the androgen precursor. Thecal cells lack aromatase, but are able to produce the androgen precursor, which is then converted to estrogen (specifically, estradiol) by the granulosa cells.
The dominant follicle continues to enlarge and secrete higher and higher levels of estrogen. Once the level of estrogen crosses a certain threshold, the feedback effect of estrogen switches from negative to positive feedback. Estrogen now stimulates the hypothalamus and anterior pituitary, resulting in a rapid rise in LH secretion called the LH surge. The LH surge is what triggers ovulation.
Following ovulation, the granulosa and thecal cells that are left
behind differentiate into the corpus luteum. The corpus luteum
secretes high levels of both estrogen and progesterone.
Estrogen and progesterone together have a negative feedback effect
on gonadotropin secretion, which limits development of other
follicles.
Refer to figure 26.12 on page 822 in Silverthorn for figures that summarize the hormonal interactions during the follicular phase, the LH surge, and the luteal phase.
A key role for estrogen and progesterone is preparing the uterus for implantation by a fertilized embryo. The lining of the uterus, or endometrium, is divided into a functional layer that changes under the influence of estrogen and progesterone, and a basal layer that regenerates the functional layer following menstruation. During the middle and late follicular phase, high levels of estrogen stimulate proliferation in the functional layer (proliferative phase). Estrogen also causes glands in the cervix to secrete a thin, watery mucus.
During the luteal phase, the high levels of progesterone inhibit proliferation, and stimulate the secretion of nutritive substances by the endometrial glands (secretory phase). Progesterone also causes the cervical glands to secrete a thick mucus that acts as a protective barrier to the uterus.
In a non-fertile cycle, the drop in estrogen and progesterone
that occurs following degeneration of the corpus luteum is what
triggers menstruation. Menstruation
is the shedding of the functional layer of the endometrium. Early
on, vasoconstriction in endometrial blood vessels causes ischemia
and tissue degeneration. Later during menstruation there is
vasodilation to cause a small amount of bleeding, along with
myometrial contractions. The bleeding and the contractions
help to expel the degenerated tissue. The first day of
menstruation coincides with the first day of the follicular phase,
and it typically lasts about 5 days. Refer to the blue/green
timeline in the figure above to see how the uterine cycle
coincides with the ovarian cycle.