Clinical Example: Heart Sounds and Valve Disorders
The heart sounds are due to the closing of the valves. As
the valve leaflets (cusps) snap shut, vibations occur in the
valves and surrounding structures, creating sounds that can be
heard through a stethoscope placed on the chest.
The first heart sound, S1 or
"lub", is due to the closing
of the AV valves, which occurs at the beginning of systole (when the ventricles begin
to contract). The second heart sound, S2
or "dup", is due to the
closing of the aortic and pulmonary valves, and occurs at the
beginning of diastole (when
the ventricles begin to relax).
Valve disorders occur when there is damage to the valve leaflets
or to the chordae tendineae. There are two general kinds of
valve disorders:
- stenosis The valve opening
is narrowed, causing resistance to flow through the valve when
it is open.
- insufficiency The doesn't
close properly, causing regurgitation of blood.
Both types of valve disorders cause turbulent flow of blood,
which makes a noise called a murmur. A useful exercise in studying
the cardiac cycle is to determine whether a murmur due to a
defective valve should be systolic or diastolic. Be sure you
can fill out the table below.
|
Systolic or diastolic murmur?
|
AV stenosis
|
|
AV insufficiency
|
|
aortic or pulmonary stenosis
|
|
aortic or pulmonary insufficiency
|
|
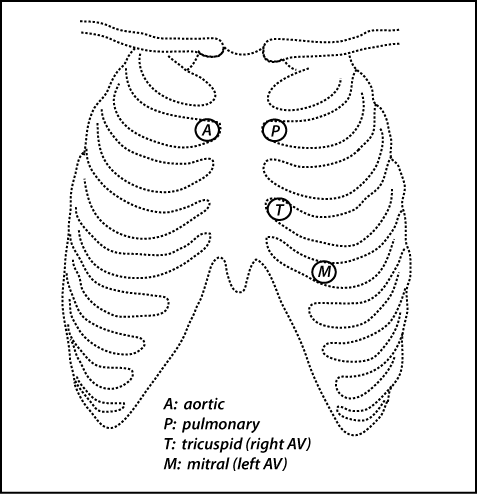 Valve
disorders can be diagnosed by careful listening to determine the
timing and location of a murmur. This technique is referred
to as auscultation. The
figure shows the locations that are best for hearing listening to
each particular valve. Note that the positions for best listening
to the aortic and pulmonary valves are opposite to what you might
think they would be based on which side of the heart the vessel
leaves. As we discuss in lecture, echocardiography
is an extremely useful modern technique that uses
ultrasound to image the heart and valves.
Valve
disorders can be diagnosed by careful listening to determine the
timing and location of a murmur. This technique is referred
to as auscultation. The
figure shows the locations that are best for hearing listening to
each particular valve. Note that the positions for best listening
to the aortic and pulmonary valves are opposite to what you might
think they would be based on which side of the heart the vessel
leaves. As we discuss in lecture, echocardiography
is an extremely useful modern technique that uses
ultrasound to image the heart and valves.
For fun, you can listen to different types of heart sounds by
going to this
page from the UW Department of Medicine.
Clinical Example: Transcatheter Aortic Valve Replacement (TAVR)
for the Treatment of Aortic Stenosis
Aortic stenosis is a
narrowing of the aortic valve. In the United States, most
patients with aortic stenosis have a degenerative disease in which
the valve stiffens and calcium deposits form on the valve
leaflets. Aortic stenosis can also be caused by a congenital
malformation where there are two valve leaflets (bicuspid
aortic valve) instead of the normal three (tricuspid aortic
valve). Aortic stenosis may also occur as a consequence of rheumatic
fever, but this is more common in the developing world.
Aortic stenosis causes symptoms when the narrowing of the valve
starts to affect blood flow. A patient with severe aortic stenosis
may experience dyspnea
(shortness of breath) upon exertion, dizziness or syncope (fainting), and angina (chest pain). These
symptoms are not specific to valve disorders, but are general
symptoms that occur in heart failure or coronary artery disease.
Severe aortic stenosis that causes symptoms needs to be
surgically treated with valve replacement, because without
treatment, symptoms worsen and mortality is quite high.
Valve replacement was traditionally done by open heart surgery,
but in the last 20 years, minimally invasive procedures have been
developed. In transcatheter aortic
valve replacement (TAVR),
a catheter is used to guide an expandable prosthetic (replacement)
valve into position. Usually, a balloon is inflated to cause
the prosthetic valve to expand. The prosthetic valve crushes
the damaged valve against the walls of the aorta, and the tissue
of the damaged, replaced valve serves to hold the prosthetic valve
in place. The femoral artery is often used as an entry point
for the catheter because it is easily accessed through the skin of
the upper thigh.
Here is a link to a short video outlining the TAVR
procedure: TAVR video (opens in a new
window)
Be sure you can trace the path that the catheter follows from
the
femoral artery to the site of the aortic valve:
femoral artery → external iliac artery
→ common iliac artery → abdominal aorta → descending
thoracic aorta → aortic arch → ascending aorta
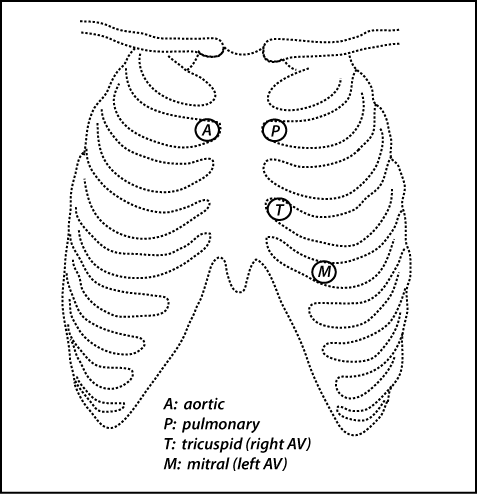 Valve
disorders can be diagnosed by careful listening to determine the
timing and location of a murmur. This technique is referred
to as auscultation. The
figure shows the locations that are best for hearing listening to
each particular valve. Note that the positions for best listening
to the aortic and pulmonary valves are opposite to what you might
think they would be based on which side of the heart the vessel
leaves. As we discuss in lecture, echocardiography
is an extremely useful modern technique that uses
ultrasound to image the heart and valves.
Valve
disorders can be diagnosed by careful listening to determine the
timing and location of a murmur. This technique is referred
to as auscultation. The
figure shows the locations that are best for hearing listening to
each particular valve. Note that the positions for best listening
to the aortic and pulmonary valves are opposite to what you might
think they would be based on which side of the heart the vessel
leaves. As we discuss in lecture, echocardiography
is an extremely useful modern technique that uses
ultrasound to image the heart and valves.