
Methods of defining prevalent fractures
Methods of defining incident fractures
Clinical significance of a mild fracture
Vertebral fractures ignored
 |
Normal vertebral dimensions Methods of defining prevalent fractures Methods of defining incident fractures Clinical significance of a mild fracture Vertebral fractures ignored |

Several studies reported the normal ratio of the anterior to the posterior height for each vertebrae. The above graph demonstrates the range seen in a reveiw of these papers.
There have been several approaches to identification of a vertebral fracture, as described in detail by Szulc. Many investigators use the cut-off of 3 standard deviations to define a vertebral fracture (as shown in the above graph). The prevalence rates vary depending on the reference range and the methodology, and there is still debate about the best way to define these fractures. The National Osteoporosis Foundation sponsored a working group about this in 1995, and suggested that more studies were needed. There are always some vertebrae that are indeterminate. It is also difficult to apply the methods when there are anatomic irregularities such as scoliosis, osteoarthritis or Scheuermann's disease.
In my clinic, I examine the vertebrae and measure the borderline ones which look like they might be compressed. If the anterior height is 20% lower than the posterior height of the same vertebra or of the adjacent ones I call it a fracture and treat the patient with an osteoporosis medication.
 The International Osteoporosis Foundation Vertebral Fracture Initiative is a new a web-based tutorial about the semi-quantitative method (with some good examples of xrays).
The International Osteoporosis Foundation Vertebral Fracture Initiative is a new a web-based tutorial about the semi-quantitative method (with some good examples of xrays).
Fracture prevalence in women with postmenopausal osteoporosis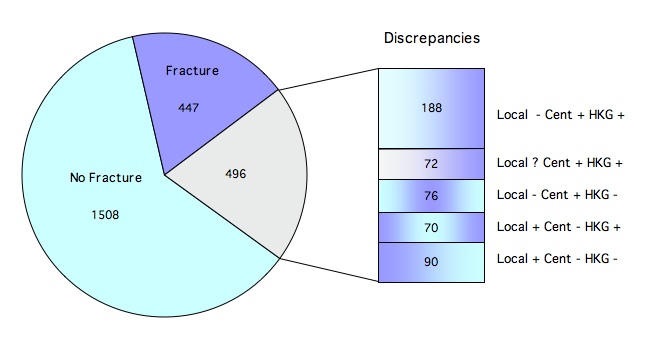
A recent article by Delmas reported radiologists opinion about whether there was a fracture from standardized xrays of patients with osteoporosis (T-score <-2.5) who were enrolled in an international study. As shown in the graph, in 20% of the women, local radiologists disagreed with radiologists in a central reading facility about whether there was a fracture. An expert radiologist (HKG) felt that 69% of the disputed xrays actually had fractures. As stated by the authors, "there will always be some discrepancies between individuals with no fractures and those with mild fractures". |
Several approaches to identification of a new vertebral fracture were described in detail by Black. They concluded that a 20-25% reduction in any vertebral height (anterior, posterior or middle) was the most practical method of assessing an incident fracture. Other studies also require a 4mm absolute loss of height compared to the previous xray. Lunt et al found that combining these criteria with a requirement that the newly fractured vertebra also met the definition of a prevalent fracture increased the specificity.
Fracture incidence over 3.8 years in European men and women older than 50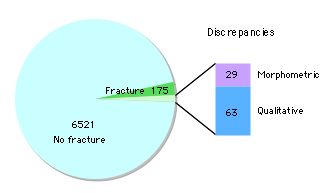
In the EPOS study of fracture incidence, two methods of defining a new fracture were based on comparison of baseline and follow-up xrays. One used morphometric measurements showing 20% loss of vertebral height plus absolute height reduction of at least 4mm. The other was a qualitative review by an expert radiologist. Both methods agreed there was a new fracture in 175 cases, and in 92 cases there was disagreement, with more cases identified by the qualitative method. |
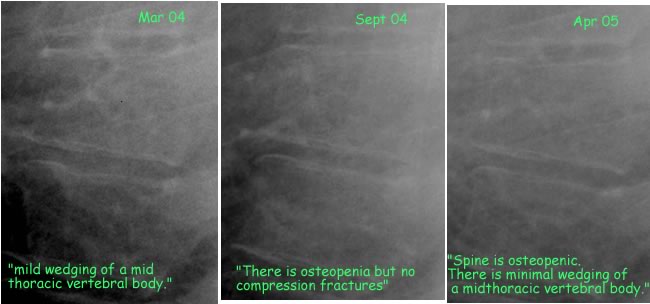
The above series of xrays was read by the same radiologist. This vertebra is truely in the "grey zone", very close to the definition of a fracture. The patient did not have any back pain. Do these mild fracture matter?
YES! The presence of a vertebral fracture increases the risk of a new fracture by about 4 times, even when adjusting for bone density.
The EPOS study (Lunt) found that overall the risk of a new vertebral fracture was 6.1 times more likely if there was a prevalent fracture. This varied with the shape of the deformities: there was no increased risk with loss of posterior height, but a 6-fold increased risk with loss of anterior plus middle height. The risk also increased with number of deformities:
| Initial deformities | Relative risk |
|---|---|
| 1 | 3.2 |
| 2 | 9.8 |
| 3+ | 23.3 |
In a clinical trial of women with osteoporosis, the spine deformity index at baseline (which measures the sum of the fractures graded according to severity) was related to the incidence of a vertebral fracture during the 3 years of the study. Those with the most severe initial fractures had the highest risk of getting a new fracture. In this study, even mild fractures increased the risk of subsequent fractures. These fractures all showed a height reduction of at least 20%.
 from Crans GG, Genant HK, Krege JH. Prognostic utility of a semiquantitative spinal deformity index. Bone 2005, article in press, with permission from Elsevier. |
In the Study of Osteoporotic Fractures ( Nevitt) there were 403 women who had a mild vertebral deformity between 2.5 and 3 standard deviations below mean. These women had an increased risk of incident vertebral fractures 4.2 times higher than women without any vertebral deformity.
| Author | Date | Chest xrays reviewed for moderate or severe fractures | N with Fx | % on report |
|---|---|---|---|---|
| Gehlbach SH | 2000 | 954 xrays in hospitalized women over 60 | 132 | 50% |
| Kim N | 2004 | 100 xrays in emergency room adults over 60 | 22 | 55% |
| Majumdar SR | 2005 | 500 xrays in emergency room adults over 60 | 72 | 60% |
These numbers are dismal enough, but even when the radiologist reported the fractures, fewer than half of the patients were prescribed treatment for their osteoporosis. We have a long way to go!
Reviewed 1/6/2011

