|
Moderate heart disease is not a risk factor for osteoporosis. The SOF study (Cummings) did find that an increased heart rate was associated with risk of a hip fracture. The HERS study (Hulley) enrolled women who already had documented coronary artery disease; these women did not have markedly decreased bone density. The overall fracture rates were 2.5%/year, which are not very high.
Patients with more severe heart failure, however, have osteoporosis. Studies of patients waiting for a heart transplant show a high incidence of osteoporosis, as well as abnormalities in vitamin D, PTH, and bone resorption. (Shane). Non-specific factors may play a role; patients with heart disease are less active, may lose weight and muscle strength, and frequently smoke cigarettes.
Associations between calcifications of the aorta and osteoporosis have been reported since the '50s. These are nicely reviewed in a paper by Watson. Arad reported that coronary artery calcifications were not related to vit D, PTH, or calcium
Several recent studies have examined vascular calcifications and their relationship to osteoporosis. Banks, Frye, M. A. and Vogt found significant correlations between aortic calcifications and bone density; in the latter studies these effects vanished when corrected for age. Kauppila has published a method for quantitating calcifications in the abdominal aorta. This approach was used to correlate bone loss from persons in the Framingham study. After 25 years of follow-up, the women in the highest quartile of bone loss had signfiicantly greater progerssion of aortic calcification. This was not seen in men, raising the possibility that estrogen status could be affecting both bones and vessels. (reported at ASBMR 1997, #174). Orwoll and Drinka also did not see a correlation in men.
Electron beam CT-scanners can quantitate calcifications of the coronary arteries. These were correlated with bone density (Barengolts). The total coronary calcium score +/- SD (relative units) was 41.9 +/- 83.1, 115.1 +/- 181.9, and 221.7 +/- 355.4 for control, osteopenia, and osteoporosis group.
Several related abstracts were presented at the 2000 ASBMR meetings:
Low Bone Mineral Density (BMD) Is Associated with Coronary Artery Calcification
D. P. Kiel examined the relation between BMD and and coronary calcification in 146 men (ages 35-76) and 157 women (ages 35-77) of the Framingham Offspring Study in whom calcification of the coronary arteries was assessed by electron beam computed tomography (EBCT). After adjustment for potential confounders in women, spine BMD (continuous variable) had the strongest inverse association with CC (p=.002). These findings suggest that BMD and CC are related processes, and that low BMD may be a marker of subclinical vascular disease.
Aortic Calcification and Rates of Bone Loss in Older Women K. E. Ensrud studied a subsample of women in the FIT study had measurements of abdominal aortic calcifications. The rate of bone loss over the next 3 to 4 years was measured in the subjects taking placebo. Raw values showed no difference in rate of bone loss in those with calcifications, but adjustment for other factors did show an enhanced loss at the hip.
Bisphosphonates prevent arterial calcifications
Price studied rats who were given large doses of coumadin or vitamin D showed that they developed arterial calcifications. If animals were pre-treated with alendronate, the calcifications did not occur.
Comment: This is not the kind of calcification seen in ordinary coronary artery disease. It is more like calciphylaxis. The effects of aminobisphosphonates on arteriosclerosis are unknown.
Related articles show that estrogens (McLaughlin) and statins both improve coronary calcifications. Williams stated: "histochemical analysis of the atherosclerotic lesions indicated that the arteries from pravastatin-treated monkeys had significantly fewer macrophages in the intima and media, less calcification and less neovascularization in the intima (p < 0.05). We conclude that compared with control monkeys, the arteries of pravastatin-treated monkeys had better dilator function and plaque characteristics". EBCT studies in humans also showed that a net reduction in the calcium-volume score was observed only in the 65 treated patients whose final LDL cholesterol levels were less than 120 mg per deciliter (3.10 mmol per liter) (mean [+/-SD] change in the score, -7+/-23 percent; P=0.01). Untreated patients had an average LDL cholesterol level of at least 120 mg per deciliter and at the time of follow-up had a significant net increase in mean calcium-volume score (mean change, +52+/-36 percent; P<0.001) (Callister)
Osteonectin
Osteopontin
Bone gla protein
* Osteoprotegerin (OPG)deficiency in transgenic mice causes premature arterial calcifications. (Bucay, et al, 1998, Genes Dev 12:1260). In humans, high levels of OPG are associated with stroke, diabetes, as well as fractures (Browner, W. S.)
Matrix gla protein deficiency in transgenic mice causes severe arterial calcifications, which suggests that this protein must be an important inhibitor of calcifications. (Luo, G.)
Nitric oxide synthetase - This is an important topic that I am planning to review. . .
This is discussed in the page about estrogen. The Women's Health Initiative results showed an increased risk of cardiovascular events and strokes in older postmenopausal women who took estrogen plus progesterone. With estrogen only, the risk of heart disease was not increased but the risk of stroke was higher than with placebo. In younger women, within a decade of menopause, the placebo group had more CHD events than the estrogen group (Rossouw JE).
A review of epidemiological literature (Grady) found a significantly reduced risk of heart disease in women who took estrogen replacement. Based on these studies, a randomized trial was performed in women who already had heart disease to see if estrogen would be effective in treatment. The Heart and Estrogen Replacement Study (HERS)
(Hulley) results, however, showed an increased risk of CHD [this stands for coronary heart disease, a rather redundant term] events in the first year of treatment with estrogen. The overall risk of CHD events over the 4 years of the study was not increased, because during the last several years the women on placebo had more events. It seems likely that the reason for the early increase was related to increased thrombosis.
Another study by Herrington found similar results. This study performed arteriography in women with coronary artery disease who were treated with estrogen or placebo, and found no benefit from estrogen therapy. The Women's Health Initiative showed an increased relative risk of heart disease in women assigned to take progestin plus estrogen. The relative hazard was 1.2 compared with placebo.
The RUTH study found no increased risk of heart disease in women taking raloxifene, compared to placebo. See the Serm page for details.
In the FIT study of alendronate, the incidence of myocardial infarctions as listed by the investigators was higher in the women taking alendronate than in the women taking placebo (relative risk 1.5). The medical records of all subjects with a serious event relating to the cardiovascular system were then copied and reviewed by a blinded, independent group of cardiologists and the events were reclassified. There was no longer any significant increase in cardiovascular side effects in the alendronate-treated women. These results have never been published, and the exact details were not given to the investigators. Since then, other bisphosphonate trials have not reported any increase in myocardial infarction. Adams reported results of a study showing that the increased in coronary artery calcifications were not significantly worse than in control women with similar baseline values.
Etidronate, the "first-generation" bisphosphonate, inhibits mineralization and animal studies showed decreased vascular calcifications with this drug (which also inhibits mineralization in the bones and causes osteomalacia which is why it is not used very often to treat osteoporosis)
Atrial fibrillation has been seen more often in the recent study of zoledronate in osteoporosis (ASBMR 2006). This effect was also seen in the FIT study but was not quite statistically significant (data not published).
The remaining approved medication for treatment of osteoporosis, has not been associated with any adverse events relating to the heart.
Parhami, F. (2001). Atherogenic high-fat diet reduces bone mineralization in mice. J Bone Miner Res 16: 182-8.
Mice susceptible to artherosclerosis were fed a high or normal fat diet, and those on the high fat diet had significantly lower bone density. This is particularly interesting in view of epidemiological studies that show a higher incidence of osteoporosis in persons with atherosclerosis, cardiovascular disease, or aortic calcifications.
I had to make a separate page about statins.
And a separate page about this rapidly growing field. leptin
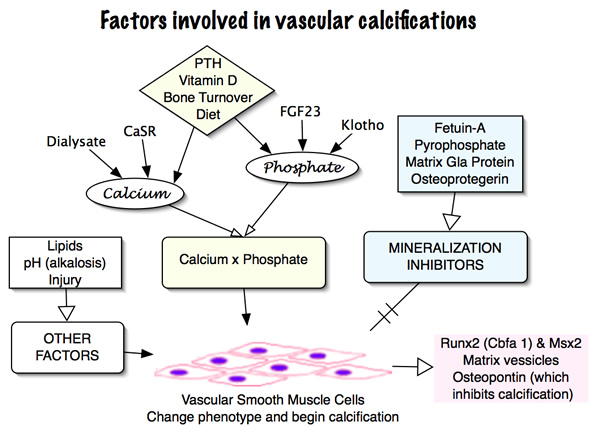
There is increasing recognition that vascular calcifications are related to mineral metabolic abnormalities in patients with kidney disease. The relative risk of death from cardiovascular disease is very high in dialysis patients, especially in the younger patients. CKD patients have low levels of fetuin-A and pyrophosphate, which are important inhibitors of calcification. Frequently they have lipid abnormalities which can cause atherosclerosis as well. The high phosphate that is a clinical problem in most patients is a very important risk factor. Some of these factors can work both ways and it is still not clear which are primary. For example, ostopontin is high in patients with vascular calcifications, but it may be a reaction to the process and not a causative factor. PTH may increase calcium which can cause calcifications, but it also increases bone turnover, and low bone turnover is associated with calcifications.
These links are not working, I need to get the newer id numbers from pub med.
Report from 1999 NIH workshop on this topic.Heart disease and osteoporosis
Banks, L. M.(1994). Effect of degenerative spinal and aortic calcification on bone density measurements in post-menopausal women: links between osteoporosis and cardiovascular disease? Eur J Clin Invest 24(12): 813-7.
Barengolts, E. I.(1998). Osteoporosis and coronary atherosclerosis in asymptomatic postmenopausal women. Calcif Tissue Int 62(3): 209-13.
Drinka, P. J.(1992). Lack of correlation between aortic calcification and bone density. Wis Med J 91(6): 299-301.
Frye, M. A.(1992). Osteoporosis and calcification of the aorta. Bone Miner 19: 185-94.
Kiel, D. P.(2000). Low Bone Mineral Density Is Associated with Coronary Artery Calcification. ASBMR 2000 Presentation Number: 1087.
Lee, M.(2000). Bone Mineral Density and Coronary Artery Calcification in Postmenopausal Women. ASBMR 2000 Presentation Number: M317.
Orwoll, E. S.(1990). The impact of osteophytic and vascular calcifications on vertebral mineral density measurements in men. J Clin Endocrinol Metab 70(4): 1202-7.
Vogt, M. T.(1997). Bone mineral density and aortic calcification: the Study of Osteoporotic Fractures. J Am Geriatr Soc 45(2): 140-5.
Watson, K. E.(1997). Active serum vitamin D levels are inversely correlated with coronary calcification. Circulation 96(6): 1755-60.
Grodstein, F.(2000). A prospective, observational study of postmenopausal hormone therapy and primary prevention of cardiovascular disease. Ann Intern Med 133: 933-41.
Herrington, D. M.(2000). Effects of estrogen replacement on the progression of coronary-artery atherosclerosis. N Engl J Med 343: 522-9.
Hulley, S.(1998). Randomized trial of estrogen plus progestin for secondary prevention of coronary heart disease in postmenopausal women. Heart and Estrogen/progestin Replacement Study (HERS) Research Group [see comments]. Jama 280(7): 605-13.
McLaughlin, V. V.(1997). Relation between hormone replacement therapy in women and coronary artery disease estimated by electron beam tomography. Am Heart J 134(6): 1115-9.
Reis, S. E.(2000). Estrogen is associated with improved survival in aging women with congestive heart failure: analysis of the vesnarinone studies. J Am Coll Cardiol 36: 529-33.
Reis, S. E.(2001). Cardiovascular effects of tamoxifen in women with and without heart disease: breast cancer prevention trial. National Surgical Adjuvant Breast and Bowel Project Breast Cancer Prevention Trial Investigators. J Natl Cancer Inst 93: 16-21.
Williams, J. K.(1998). Pravastatin has cholesterol-lowering independent effects on the artery wall of atherosclerotic monkeys. J Am Coll Cardiol 31(3): 684-91.
Callister, T. Q.(1998). Effect of HMG-CoA reductase inhibitors on coronary artery disease as assessed by electron-beam computed tomography. N Engl J Med 339(27): 1972-8.
Browner, W. S.(2001). Associations of serum osteoprotegerin levels with diabetes, stroke, bone density, fractures, and mortality in elderly women. J Clin Endocrinol Metab 86: 631-7.
Luo, G.(1997). Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature 386: 78-81.
Updated 4/29/07, but still needs work and current references