
 |
|
The most current recommendation from the the U.S. Preventive Services Task Force is to avoid calcium supplements. Instead calcium should come from food. The Institute of Medicine recommends that women should take 1200mg of calcium a day (total amount including food) for best bone health. The European Society for Clinical and Economic Aspects of Osteoporosis recommends a calcium intake of 1000mg/day (Rizzoli, 2014)
It is important to remember that these new reports are largely still based on the Women's Health Initiative, which did not show a benefit for fracture prevention. However, the women were already taking an average of 1100mg of calcium a day, so an extra 1,000 mg did not help. The bones need an adequate amount of calcium, but once that is achieved, extra will not go into the bones. A report by Prentice examined only the women who were not taking extra calcium, and after 5 years they did show fewer hip fractures than those with placebo.
A large study of over 100,000 Swedish men and women who filled out food frequency questionnaires in 1997 showed that those who drank more milk had a higher fracture rate and higher mortality, but those who ate more yogurt and cheese had fewer fractures and lower mortality. This is the first large study to suggest that the kind of dairy product makes a difference. Perhaps the lactose in milk is the reason for these findings. Yogurt does not have lactose and is good for people with lactose intolerance (Michaelsson, 2014)
Most of my patients think calcium goes to the bone, and that is partly true. The bones do need calcium to repair damage and maintain strength. But excess calcium will not help the skeleton. The bones only take what they need, and the rest must be removed by the kidney, or it will accumulate in the wrong places (joints, blood vessels, kidneys themselves). Another factor to consider is that about 80% of the calcium you eat stays in the intestines, where it prevents absorption of oxalate. We take this into account when we recommend about 1000 to 1200mg/day of calcium.
Some investigators have analyzed clinical trials and found an increased risk of cardiovascular disease from calcium supplements, and suggest that a balanced diet should be the source of calcium nutrition (Reid, 2015). This is currently a controversial topic - here is the other point of view by Lewis.
After reading these article and recommendations, I think that adult men and women should aim for a total calcium intake of 1,000 to 1,200 mg/day. It would be best to get this from dietary sources, especially yogurt and cheese and high-calcium vegetables. The average ordinary diet (without dairy) contains about 200mg of calcium, so adding three servings of calcium-rich foods a day will satisfy the requirements. If supplements must be used, it seems best to eat them with the food and in small doses (200 to 300 mg).
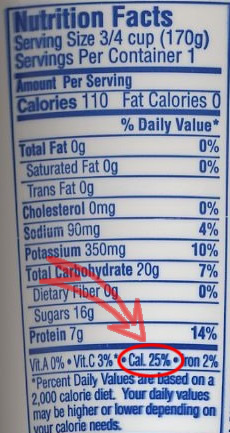 |
Nutrition LabelsFood labels show the amount of calcium per serving. These are based on the RDA of 1000mg/day. Add a zero to the %RDA for calcium to calculate the mg of calcium. For example, this label from a yogurt container shows that the calcium is 25% of the RDA, which is 250mg.The U.S. Department of Agriculture has a very detailed list of foods containing calcium, ranked in order of calcium content. Here is the pdf file of the foods with calcium. Just be aware that some sources do not have bioavailable calcium, and some of the serving sizes are larger than usual. You can also check calcium content of any food by searching the UDSA Nutrient Data Laboratory. Here is a simple list you can print: calcium content of some foods. |
If it is just too difficult to get enough calcium in foods, then small doses of these supplements can be added and taken with food. There is still controversy about safety of calcium supplements, and until more information is available it would be wisest to limit daily supplements to 600mg/day and then eat two servings of calcium-rich foods. Probably it would also be better to take pills twice a day, and cut the Caltrate or Os-Cal in half.
There are hundreds of brands and the labels don't have to say what else is in the tablets, the pills don't have to dissolve, federal agencies do not test these pills, they are not treated like medicines. The FDA is restricted by a federal law that prevents it from subjecting supplements to the strict approval process applied to prescription drugs (there have been articles about this in the March 2015 New York Times). Therefore, use only a brand that is reliable, as shown in this figure. More expensive supplements with added ingredients do not result in additional benefit and they are a waste of money.

| BRAND | Calcium per pill |
cents/pill | cents/day | Vitamin D per pill |
Comment |
|---|---|---|---|---|---|
| TUMS | 300 | 4 | 8 | none | chew with food |
| Caltrate | 600 | 9 | 9 | 800 IU | take with food |
| OsCal | 500 | 12 | 12 | 600 IU | take with food |
| Viactiv | 500 | 12 | 12 | 500 IU | avoid if you're on coumadin |
| Citracal | 315 | 9 | 18 | 250 IU | not for people with kidney disease |
This table shows amount of ELEMENTAL calcium per tablet. Sometimes the labels are confusing; they give the calcium per serving instead of per tablet. For example, the label on Citracal caplets says each serving contains 630 mg of calcium, but a serving is 2 tablets so each pill has 315mg of calcium. TUMS labels are also confusing; the number is the weight of the pill, not the amount of calcium. Therefore, regular TUMS weighs 500mg and contains 200mg of calcium; extra-strength TUMS weighs 750mg and contains 300mg of calcium, and ultra TUMS weighs 1000mg and contains 400mg of calcium.
Calcium carbonate is the most cost-effective source of calcium. The intestinal absorption of calcium citrate and calcium carbonate is similar except when there is no acid in the stomach (Heaney.) Some studies show a benefit with calcium citrate (van der Velde.)
Not all calcium preparations are absorbed equally, and one of the reasons is that they have different rates of dissolution. It is less expensive to manufacture calcium carbonate in a compact form that will not readily dissolve. The dissolution of 27 brands of calcium varies from 33% to 75% (Brennan.) Chewable tablets are a safe bet.
I was skeptical about the importance of dissolution until one of my patients told me that she had forgotten to take her calcium tablets, which she purchased from a health-foods store. She put them in the pocket of her apron, and discovered them there after the apron had been through the cycles on the washer and the dryer!
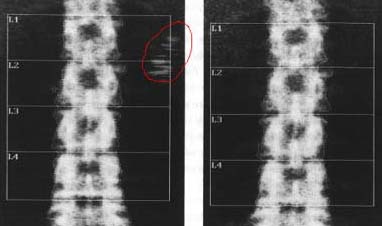 |
Another patient used a calcium supplement from a health food store, and, when she came in to have her bone density measured, densities were seen near the spine, shown with red circle. These changed position after a couple of hours, and were not seen on a scan several days later (after she switched to a chewable form of calcium). |
Side effects from a reasonable dose of calcium (up to total calcium intake of 1000 mg/d) are very low. Some patients find that calcium makes them constipated. A study by Lewis,2012 found that calcium increased constipation and other gastric problems. To help prevent constipation, don't take more calcium than necessary, increase intake of fruit juices and water, try getting calcium from food sources instead of tablets, take calcium with magnesium, or try calcium citrate or calcium chews. Gastritis is occasionally seen, which might be caused by taking calcium carbonate between meals, thus stimulating rebound acid production.
Very high intakes of calcium could lead to alkalosis (the "milk-alkali syndrome").
Calcium supplements may increase the risk of kidney stones, especially if the intake is over 2,000mg/day. On the other hand, a large survey in 45,619 men showed that those with the lowest dietary calcium had the most kidney stones. This is because the most common kind of kidney stone is caused by oxalate, and calcium inhibits the oxalate absorption from the intestines. A similar large observational study in women also found that there were more kidney stones in women with low calcium intakes (Sorensen). Old-fashioned advice about avoiding calcium increases the risk of both osteoporosis and another kidney stone! Decreasing salt and protein may also help decrease the incidence of calcium-oxalate kidney stones. Patients with hypercalciuria and low bone density can be treated with low doses (12.5 to 25mg/day) of thiazide, using potassium bicarbonate as necessary to keep serum potassium normal.
A study by Bolland suggested that calcium supplements could increase the risk of heart attacks. There were 1,400 women in this clinical trial, followed for 5 years. This side effect was not seen in a much larger study by Jackson and investigators for the Women's Health Initiative, which enrolled 36,282 women and studied them for 7 years. Also, a subset of patients received cardiac CT scans to look for calcifications in the coronary arteries, and there was no increase in the group who had received calcium (Manson). There are also some studies suggesting increased calcifications in the blood vessels with too much supplementation, but a recent review by Spence did not find a consensus that this was true. A meta-analysis, also by Bolland, did find a mild increased risk of myocardial infarction in those taking calcium supplements. This included 15 clinical trials of calcium (but not with vitamin D). Of note, there was no risk in the patients whose total calcium intake was lower than 1400 mg/day. I have been recommending a total intake of 1200mg/day for fracture prevention, based on my review of studies about osteoporosis, so this paper (even if it is true) does not change my recommendations.

Dietary protein and caffeine can cause small increases in urine calcium. These effects can be measured and are statistically significant, but become clinically important only at large intakes. In fact, a latte will result in positive calcium balance! 👍
 Calcium absorption is inhibited by fibers and oxalates in the diet. For example, although the calcium content in spinach is high, almost none gets absorbed. The spinach is not harmful, but you can not count it as a good source of calcium. Kale, however, has easily absorbable calcium! This was shown from an elegant study. The scientists grew kale and spinach in hydroponic solutions with radioactive calcium. Volunteers who ate the spinach or kale had measurements of radioactive calcium from blood, urine, and stool, so it was possible to tell how much calcium was absorbed and how much just went right through! (Heaney)
Calcium absorption is inhibited by fibers and oxalates in the diet. For example, although the calcium content in spinach is high, almost none gets absorbed. The spinach is not harmful, but you can not count it as a good source of calcium. Kale, however, has easily absorbable calcium! This was shown from an elegant study. The scientists grew kale and spinach in hydroponic solutions with radioactive calcium. Volunteers who ate the spinach or kale had measurements of radioactive calcium from blood, urine, and stool, so it was possible to tell how much calcium was absorbed and how much just went right through! (Heaney)
A meta-analysis by Tang found 29 randomized trials of calcium, with or without vitamin D. There was an overall 12% reduction in the risk of osteoporotic fractures with calcium. Addition of vitamin D did not make very much difference. The benefit was greatest in the people who had lowest calcium intake, were elderly, and had high compliance rates.
The Women's Health Initiative study (Jackson) did not find that calcium supplementation helped prevent fractures, but there was an increased risk of kidney stones. The average calcium intake at the baseline was 1148mg, which was already at the recommended level. The women took an extra supplement of 1,000 mg/day with 400 units of vitamin D. That means those in the calcium group were taking over 2,000 mg/day of calcium. Perhaps that is why the calcium did not seem to help. We need enough calcium, but extra calcium does not help the bones, it just stresses the kidneys. The women who were not already taking calcium supplements did show a reduction in the rate of hip fractures.
A study of 76,507 postmenopausal women from the NORA study (Nieves) estimated calcium intake from a questionnaire and asked about fractures 3 years later. The calcium intake was not related to the risk of fractures. Those with life-long highest calcium intakes, however, did have higher bone density. The average calcium in the diet was 600mg/day and the average total calcium intake (food plus supplement) was 900mg/day.
There have been many older randomized trials (Excel file) of calcium supplementation, but they have not been large enough to determine effect on fractures, and effects on bone density were modest. Several studies have randomly assigned menopausal women to placebo, calcium, or estrogen; those on estrogen did not lose bone, those on calcium lost some bone, and those on placebo lost the most. More contemporary studies have also given vitamin D and are listed in the next page.
The major mechanism whereby calcium effects bone is probably through inhibition of PTH secretion. Calcium could alter the physical-chemical properties of the bone mineral. With inadequate calcium, the bone is not optimally mineralized. Direct effects of calcium on the calcium receptor could also play a role.
Updated 3/31/19

