Spinal Reflexes
In a reflex, a stimulus to a sensor leads to a response in an
effector. The neural pathway controlling the reflex is
called the reflex arc.
The reflex arc consists of the afferent pathway, a portion of the
central nervous system, and an efferent pathway. Spinal
reflexes are often used in neurological testing because they are
simple, reproducible behaviors.
The Stretch Reflex
The stretch reflex is a commonly tested reflex in medical
practice. People are most familiar with this reflex at the
knee. The physician uses a reflex hammer to rap on the patellar
tendon. As a result of activation of the reflex arc, the lower leg
kicks forward. Technically speaking, the behavior that
occurs is extension of the leg at the knee.
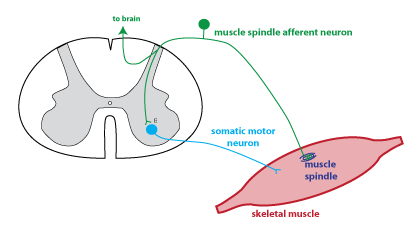 The figure to the right
shows the circuitry underlying the stretch reflex. The rap
of the tendon acts to stretch the muscle. This activates
sensors called muscle spindles.
Muscle spindles are small sensory organs that are scattered
throughout the body of the muscle, in parallel to the muscle
fibers.
The figure to the right
shows the circuitry underlying the stretch reflex. The rap
of the tendon acts to stretch the muscle. This activates
sensors called muscle spindles.
Muscle spindles are small sensory organs that are scattered
throughout the body of the muscle, in parallel to the muscle
fibers.
Muscle spindles are proprioceptors
(see below) that monitor muscle length.
The stretch of the muscle causes increased action potentials in
the muscle spindle afferent
(green). The muscle spindle afferent makes a direct synaptic connection
to a somatic motor neuron
that innervates the same muscle. Thus when the muscle
spindle afferent is activated by stretch, it excites the somatic
motor neuron to cause contraction in the same
muscle.
Returning to the test described in the first paragraph, the rap
on the patellar tendon lengthens muscles in the quadriceps group
(located on top of the thigh). The reflex response is
contraction of these muscles, i.e. extension of the lower
leg. The quadriceps stretch reflex is the one most often
tested in a general physical exam, but all the muscles have
stretch reflexes.
Where are the cell bodies of muscle spindle afferents located?
answer
Where are the cell bodies of somatic motor neurons located?
answer
Proprioceptors
"Proprio-" means "self", and proprioceptors such as the muscle
spindle provide information that is intergrated in the brain to
provide information about the position of the limbs in space (note
that the muscle spindle afferent sends an axon branch to the
brain). Muscle spindles provide information about muscle length. Another type
of proprioceptor is the Golgi tendon organ. Golgi
tendon organs are located in the tendons and are best stimulated
when the muscle pulls on the tendon. Thus, the Golgi tendon
organ provides information about muscle tension.
Reflexes in Neurological Testing
The test of the stretch reflex is used to evaluate the elements
in the reflex arc, but also higher motor control centers in the
central nervous system. If the stretch reflex is weak or
nonexistent, that indicates that there is damage to the neurons in
the reflex arc.
Spinal neurons involved in the stretch reflex receive input from
the brain, so brain and spinal cord damage can affect the size of
the stretch reflex. Recall that the upper
motor neurons are neurons whose cell bodies are
located in the primary motor cortex,
and whose axons descend to the spinal cord via the corticospinal tract. Upper
motor neuron input has a largely inhibitory effect on the stretch
reflex. Thus, upper motor neuron
disorders are characterized by hyperreflexia (exaggerated
reflexes) and hypertonia
(increased muscle tone).
Another abnormal behavior associated with an increased stretch
reflex is called clonus.
Clonus is an oscillatory movement, usually observed at the ankle
joint. A muscle stretch causes a beating motion of the foot
due to alternating contractions of antagonist muscle groups. The
video clip in this article shows sustained clonus in a patient
who had suffered a stroke ("Clonus after a Stroke" (2013) New
England Journal of Medicine 368:e2). Clonus, hyperreflexia,
and hypertonia are considered positive signs associated
with upper motor neuron disorders (see Brain
Anatomy:
Clinical
Examples).
Another reflex that can reveal damage to the upper motor neurons
is the Babinski reflex (also called the plantar reflex).
To test this reflex, a blunt object, such as the handle of the
reflex hammer, is run along the lateral sole of the foot, moving
from the heel in the direction of the toes. If there is no damage
to the corticospinal tract, the patient will curl the toes.
If there is damage to the corticospinal tract, the response is
extension of the big toe and fanning of the other toes. This
is known as a positive Babinski sign. Infants also have a
positive Babinski sign due to the fact that the corticospinal
tract is not yet fully myelinated.
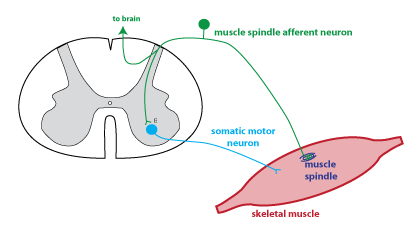 The figure to the right
shows the circuitry underlying the stretch reflex. The rap
of the tendon acts to stretch the muscle. This activates
sensors called muscle spindles.
Muscle spindles are small sensory organs that are scattered
throughout the body of the muscle, in parallel to the muscle
fibers.
The figure to the right
shows the circuitry underlying the stretch reflex. The rap
of the tendon acts to stretch the muscle. This activates
sensors called muscle spindles.
Muscle spindles are small sensory organs that are scattered
throughout the body of the muscle, in parallel to the muscle
fibers.