X-ray gallery
Surveys that viewed X-rays
Database studies
Incidence
Background incidence
Theories about etiology
Management
My invited papers that were rejected
References
 |
Features X-ray gallery Surveys that viewed X-rays Database studies Incidence Background incidence Theories about etiology Management My invited papers that were rejected References |
By May 2011 there have been 56 papers describing a total of 329 cases. Through 2009 there were data about 85 individual cases. Their features are described in the table below. The second column is from a case series by Isaacs (40 patients).
| Subtrochanteric or shaft (diaphyseal) part of the femur | Isaacs series |
|---|---|
| Minimal or no trauma (all) | 22% sponteneous |
| Frequently preceded by weeks to months of thigh pain | 71% |
| Bilateral in 47% of cases, in similar location | 44% |
| Patients younger than typical femur fractures (mean age 65) | 73 yrs |
| Bisphosphonate use longer than 5 years in 77% of cases | mean 7.1 yrs |
| Frequently another cause of osteoblast suppression | |
| Bone density not severely decreased | |
| X-rays show thick cortices, especially on lateral side (all) | |
| Often a "beaking" that resembles a stress fracture | |
| Fractures may not heal very well | |
| Femur more likely to crack during surgery |
You can download a list of my notes on these publications
 EXCEL FILE ABOUT ATYPICAL FRACTURES
EXCEL FILE ABOUT ATYPICAL FRACTURES
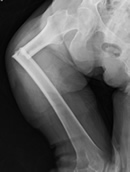
It is important to recognize the appearance of these lesions that precede a fracture. These patients were on long-term bisphosphonates and had some thigh pain, then suffered a broken femur after a minor fall. Click on the thumbnail go to the full image (use your browser "back" button to return).
Goh SK, from Singapore, identified 13 non- traumatic subtrochanteric fractures from a review of medical records over a 10 month period. Nine of the patients were taking bisphosphonates, and they were younger, had higher bone density, and thicker bone on the radiographs of the femur. During the next 10 months 8 more patients taking alendronate had non-traumatic subtrochanteric fractures
The second series included all low-energy subtrochanteric fractures seen over 5 years from a large New York hospital (Neviaser AS,Lenart BA) There were 69 patients, and 36% of them had been taking alendronate with mean duration of 6.2yrs. Twenty patients had an unusual radiographic appearance of thick cortices and a unicortical beak; 19 of them were taking alendronate.
Giusti reviewed 906 X-rays of surgical femur fractures and found 63 low-energy shaft fractures of when 10 had an atypical appearance. Half had bisphosphonate exposure, compared with 2/53 patients with ordinary femur fractures.
Isaacs, from Australia, reviewed all cases of low-energy femoral shaft fractures from 1995 to 1997 and then from 2007 to 2009. None of the early subjects had the atypical appearance. Of 79 later cases, 41 had an atypical x-ray, and they all had been taking a bisphosphonate.
Banffy also searched all cases in their institution in Boston and found 34 cases with atypical x-ray appearance and they had all been taking a bisphosphonate.
 From Sweden, Schilcher reviewed records from all women older than 55 in 2008. Using registry data, there were 1315 diaphyseal fractures, but after radiographic classification there were only 322. Of these, 59 had an atypical appearance, which was seen in 13 of 1,437,820 nonusers and 46 of 83,311 bisphosphonates users (age-adjusted relative risk of 47). 85% of these occurred after more than 2 years of bisphosphonate use. The incidence was 8.5 per 10,000 patients/year with over 2 years of exposure.
From Sweden, Schilcher reviewed records from all women older than 55 in 2008. Using registry data, there were 1315 diaphyseal fractures, but after radiographic classification there were only 322. Of these, 59 had an atypical appearance, which was seen in 13 of 1,437,820 nonusers and 46 of 83,311 bisphosphonates users (age-adjusted relative risk of 47). 85% of these occurred after more than 2 years of bisphosphonate use. The incidence was 8.5 per 10,000 patients/year with over 2 years of exposure.
At Kaiser in California, we have been reviewing X-rays of all patients with a fracture in the lower part of the femur, and 130 of 135 were taking bisphosphonates. The longer the duration of use, the greater the risk of fracture, with a significant increase after 5 years. This data has been presented at the ASBMR and submitted but not yet accepted for publication.
These studies use codes to identify cases, without looking at the x-rays. We recently published a paper which found limited accuracy using ICD-9 codes (Spangler L)
A study by Abrahamsen casts some doubt about how often subtrochanteric fractures are related to bisphosphonates.
 The Danish hospital registry identified all cases. The alendronate-treated patients had higher incidence of both hip and subtrochanteric or shaft fractures, and the proportion of hip fractures was similar for both groups. It is interesting that the alendronate-treated patients actually had higher fracture rates even though they were matched. There could have been some other factors that caused physicians to give the bisphosphonates to the patients in the first place. The registry-based analysis does not allow for any details about the patients or their clinical symptoms. The investigators did not view the x-rays, and not many people took the bisphosphonates for more than 6 years. Furthermore, all of the people in the study already had one fracture, so those whose first fracture was a femur fracture would not have been included.
The Danish hospital registry identified all cases. The alendronate-treated patients had higher incidence of both hip and subtrochanteric or shaft fractures, and the proportion of hip fractures was similar for both groups. It is interesting that the alendronate-treated patients actually had higher fracture rates even though they were matched. There could have been some other factors that caused physicians to give the bisphosphonates to the patients in the first place. The registry-based analysis does not allow for any details about the patients or their clinical symptoms. The investigators did not view the x-rays, and not many people took the bisphosphonates for more than 6 years. Furthermore, all of the people in the study already had one fracture, so those whose first fracture was a femur fracture would not have been included.
A subsequent study by Abrahamsen examined 39,567 patients who used alendronate and found an incidence of 0.31% per year for subtrochanteric or shaft fractures. The rate in controls was 0.13%. They did not see any increased risk in the patients who had received 9 years of treatment. Again, they did not examine the x-rays. Another study from Denmark by ve found that the patients who used bisphosphonates had more diaphyseal femur fractures than controls both before and after medication use, without an increase with longer duration. This study also did not look at the x-rays
A similar study was recently presented at the ASBMR using the Veteran's Administration database (Saord). There are several other studies that have not shown an increase in the rate of subtrochanteric fractures which might be expected if these were increasing due to bisphosphonates (Nieves JW, Adachi, Curtis)
Park-Wyllie did a case-control study in all women who started alendronate when they were older than 68, and compared the incidence of diaphyseal femur fractures in those who took bisphosphonates longer than 5 years to those who stopped before 3 months. The odds ratio was 2.74 (1.25-6.02) which suggested that these patients with long-term use had a greater chance of a femur fracture. After 5 years of bisphosphonate, the absolute risk was 0.13% in the next year. This study did not review x-rays. Importantly, the women had to start treatment when they were older than 68, so the youngest patients with 5 years of treatment would be 73 years, which is older than the average age from other reports.
At this time the incidence is not known. One paper estimated it was 1/1000 in long-term users (Schilcher J). A subsequent study from Sweden found 0.8 per 1000 after 2 years of use.
There have always been fractures of the femur, even before bisphosphonates. Here is a graph of data from four studies:
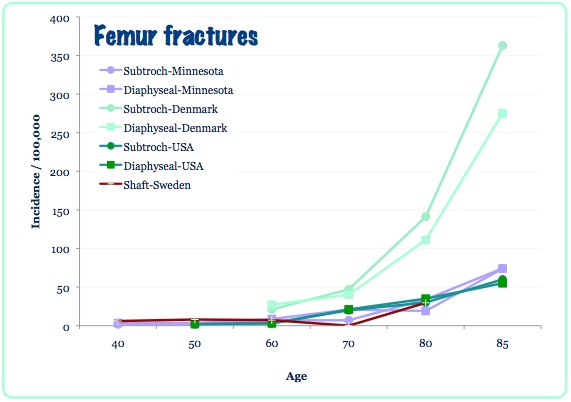
The first (purple) was in women from Rochester, Minnesota, between 1965 and 1984 (Arneson). Of these, 58% were caused by severe trauma. The second study (red) showed rates in the 1980's in Sweden (Bengner). The third (dark green) was by Nieves, who used discharge database surveys to look at incidence of subtrochanteric fractures in the USA. The rates were stable from 1996 to 2006 and are similar to those from Minnesota; the plot shows data for the women. The rates from a recent Danish database reported by Abrahamsen are higher in the older group; 38% were low energy and 41% unknown trauma.
In Finland, from 1985 to 1994, low-trauma fractures of the femoral shaft were seen in 7.8 per 100,000 people older than 60. The majority were the spiral type (Salminen). In the elderly, these femur fractures are about 1/10 as common as hip fractures.
Bone biopsies often show very low bone formation, but some have not seen this. Biopsies at the site of the fracture are usually done to rule out cancer or other pathology, and there have been mixed reports about whether osteoclasts are increased.
Perhaps the suppressed bone turnover allows accumulation of micro-cracks, which then can result in a stress fracture.
Many features of these fractures resemble the "march fractures" seen in military recruits. Perhaps these younger women with less severe osteoporosis are more active and thus are accumulating damage at a higher rate than the more usual elderly woman with severe osteoporosis.
There are also some abnormalities in the chemical crystal structure of the bone mineral that might make the bone more brittle (ASBMR09 Boskey).
At this time there is no consensus about management. Several recent studies have shown a high risk of compete fracture if there is a stress fracture with a "dreaded black line" (Ha YC, Koh JS). For example, Banffy MB had 12 patients with non-displaced stress fractures. Six had a rod, six were followed, and 5 of them went on to have a complete fracture.
There is some rationale for treating with teriparatide. There was one case report of successful healing ( Gomberg SJ). This medication helps to heal stress fractures. However, in view of the high risk of complete fractures, it may not be safe to use this drug alone (without surgery) in patients who already have a fracture line. It is probably a good adjuvant medication, and there is a possibility it could reduce the risk of another fracture. Teriparatide is a good therapy for "ordinary" stress fractures( Sloan AV.)
A biopsy study in persons who took teriparatide found that microcrack damage was significantly improved in the patients who had previously been taking alendronate (Dobnig H).
 in Dobnig H, Stepan JJ, Burr DB, et al. Teriparatide Reduces Bone Microdamage Accumulation in Postmenopausal Women Previously Treated with Alendronate. J Bone Miner Res 2009, online May 19. Used with permission from ASBMR
in Dobnig H, Stepan JJ, Burr DB, et al. Teriparatide Reduces Bone Microdamage Accumulation in Postmenopausal Women Previously Treated with Alendronate. J Bone Miner Res 2009, online May 19. Used with permission from ASBMR
Sept 2011 A review in the Cleveland Clinic Journal of Medicine (pdf file).
In 1997 I was asked by the editor of the New England Journal of Medicine to write an editorial about alendronate. This was initially accepted, but at the last minute it was cancelled.
In 2009 the editor of the Journal of Clinical Metabolism and Endocrinology invited me to write an article about the approach a patient who had been taking long-term bisphosphonates. However, the reviewers thought it was too biased, and the paper was rejected.
 .pdf file of 2009 rejected paper |  .pdf file of 1997 rejected paper |
The reviewers of the paper said: "This is an opinion paper, based upon a very sparse literature that calls attention to an exceedingly rare event recently associated with long-term bisphosphonate therapy. There are many issues that although mentioned are not dealt with in depth or in a scholarly manner. The literature cited is selective and the interpretation is even more so."
" The abstract suggests a very negative view about continuing bisphosphonate therapy beyond 5 years. This unqualified view, repeatedly emphasized in a discussion that is rather loose, rambling and not consistent, runs counter to many experts and also much literature arguing the other view."
"This paper allows the author to express her practice pattern to stop BP treatment in all patients after 5 years. She readily admits that this action is not based on any solid evidence, but rather her concerns about potential harm. . . The paper would be better if it focused on patients who have done well on treatment."
"I think it is premature to go into detail here. There is evidence that these fractures are not related to bisphosphonate treatment but rather an uncommon fracture due to osteoporosis."
The journal that rejected my review published a different one: Watts NB. Long-Term Use of Bisphosphosphonates in Osteoporosis. J Clin Endocrinol Metab, 2010. They concluded:
"Since their initial introduction in the United States
in 1995, questions have been raised about their association
with possible side effects (ONJ, musculoskeletal pain,
atrial fibrillation, atypical fractures, esophageal cancer)
that appear to be rare and may not be causally related."
In September 9, 2011 the FDA will hold a meeting about this topic, and background material can be found at this site.
In the media:
A national news broadcast about this on ABC.
Two local reports (Seattle) and interviews with Dr. Ott:
KING,
KOMO

