
Pleural Effusions
Case 4 Answers
A 34 year-old woman with a history of heavy alcohol use presents to the emergency room complaining of increasing shortness of breath and right-sided chest pain. Her past medical history is remarkable for several prior episodes of pancreatitis, likely secondary to her chronic alcohol use. A chest x-ray is performed and is shown below:

She initially undergoes thoracentesis for symptom relief but studies are not performed on the fluid. A repeat thoracentesis is then performed and 2 liters of serosanguinous fluid are removed. The pleural fluid studies reveal LDH 894 (serum value 175), total protein 3.6 (serum value 5.3), WBC 4000 with 90% eosinophils. The gram’s stain is negative.
How would you interpret the results of the pleural fluid analysis?
The LDH value is well above the upper-limit of normal for serum, while the pleural fluid: serum LDH ratio is > 0.6 and the pleural fluid: serum ratio is > 0.5. This effusion should therefore be classified as an exudate.
What do you make of the high percentage of eosinophils in the pleural fluid?
Although the presence of eosinophils in blood is extremely helpful from a diagnostic standpoint, they have much less diagnostic utility when they are present in pleural fluid. The leading causes of pleural fluid eosinophilia are air in the pleural space (eg. prior pneumothorax or previous thoracentesis) or blood in the pleural space (eg. hemothorax from trauma). In her case, they are probably due to the prior thoracentesis. The old saw used to be that high eosinophil counts in the pleural fluid were highly suggestive of malignancy but subsequent case series showed that malignancy accounted for only 11-30% of effusions with > 10% eosinophils. The list of other diagnoses that can cause eosinophil rich pleural effusions is very large but the most common causes include parapneumonic effusions, tuberculosis, pulmonary embolism, lymphoma, eosinophilic pneumonia, pancreatic pseudocysts and a host of others. Eosinophils can be present in transudative or exudative effusions. Large numbers of eosinophils in the pleural fluid are not typical for the type of effusion this patient was found to have.
What additional tests should you order on the pleural fluid?
In a patient with a history of multiple episodes of pancreatitis related to alcohol use you should consider ordering an amylase level in the pleural fluid. Other potential tests you can order on exudative effusions of unclear etiology include a rheumatoid factor to rule out chronic rheumatoid pleurisy, ANA to rule out lupus pleuritis, adenosine deaminase to rule out tuberculosis and perhaps a pH and glucose as very low levels on those two tests might narrow your differential a bit (this is discussed in a later case).
A CT scan of her chest and abdomen is performed. The scan reveals the presence of a possible pancreatic cyst, shown below. This prompts the physicians to order a pleural fluid amylase, which comes back at 4855 (normal < 20). How does this change your differential diagnosis?
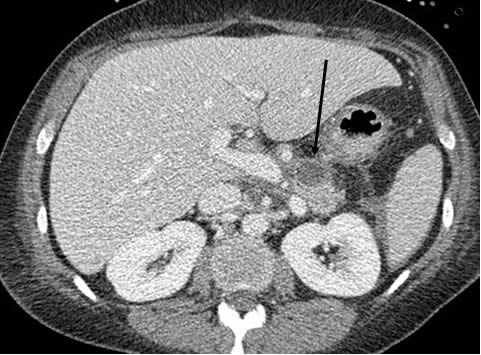
The arrow in the scan points to a pancreatic pseudocyst from her prior episodes of pancreatitis. The pleural fluid amylase level is markedly elevated. The leading items on the differential diagnosis for an elevated pleural fluid amylase is short and includes acute pancreatitis, chronic pancreatitis (pleural fluid tracks to the pleural space from a pancreatic pseudocyst), malignancy and esophageal rupture. Less common causes include ovarian adenocarcinoma, ruptured ectopic pregnancy and chronic lymphocytic leukemia. In this patient’s case the presence of a pancreatic pseudocyst makes it highly likely that she has a pancreatico-pleural fistula with fluid tracking from the pseudocyst to the pleural space.
How can you distinguish between pancreatic and other causes of amylase-rich pleural effusions?
In amylase rich pleural effusions due to pancreatic causes, the amylase is largely the pancreatic isoenzyme while in cases of malignancy or esophageal rupture, it is usually the salivary isoenzyme that is present. The degree of amylase elevation is also usually much higher in pancreas-related processes.
What can you do to manage this patient’s pleural effusion?
Her effusion is due to the fact that fluid is tracking from the pancreatic pseudocyst to the pleural space. The initial management strategy is to promote decompression of the pseudocyst by allowing it to drain in another direction. To facilitate this, patients typically undergo ERCP with stenting of the pancreatic duct, which allows fluid to drain from the pseudocyst to the intestinal tract rather than to the pleural space. If this fails, then other surgical options are considered.
UW School of Medicine : School of Medicine Mission
Copyright and Disclaimer : Credits and Acknowledgements