
 |
 Khosla S. Update in male osteoporosis. J Clin Endocrinol Metab 2010;95(1):3-10. This is an excellent new overview of this topic.
Khosla S. Update in male osteoporosis. J Clin Endocrinol Metab 2010;95(1):3-10. This is an excellent new overview of this topic.
One fifth of hip fractures occur in men. The exponential increase in hip fractures with age is seen in both genders, but the rise occurs about 10 years later in men than in women. Males lose bone density with aging, but because males begin with a higher bone density, they reach osteoporotic levels at an older age than females. Also, men do not undergo the rapid bone loss associated with menopause. By the age of 90, about 17% of males have had a hip fracture, compared to 32% of females. The incidence and prevalence of fractures for both men and women are shown in the demographics section.
Bone density predicts fractures in men and in women. The relationship between bone density and fracture risk for men is shown in the updated page about bone density and fracture risk. There is some discrepancy between studies. The international meta-analysis shows that men and women will experience the same risk of hip fracture if they have the same age and femoral neck bone density. Note that the new WHO fracture risk calculator uses T-scores based on female reference data (details on the fracture risk calculator.) The MrOs study, in the USA, however, finds that women have a higher over-all fracture risk even when they have the same age and bone density at the total hip.
Basic prevention is the same in men as in women. Both men and women need adequate calcium, vitamin D, exercise, optimal weight, and should not smoke cigarettes.
Hypogonadism is an important cause of osteoporosis in men. The recent MrOS study found that men whose serum bioavailable testosterone was in the lowest quartile had a 2.5 times increased risk of non-spine fractures compared with the highest quiartile. Bioavailable estrogen also was related to fractures. Interestingly, the estrogen was related to bone density, so the fracture effect was not seen after adjustment for bone density. The testosterone risk was independent of bone density - in fact, it was not even correlated to bone density. Other studies, however, have found a relationship between testosterone levels and bone density.
Also men clinically diagnosed with hypogonadism consistently have low bone density. Measurements of testosterone in men with hip fractures show low levels of free testosterone. Bone biopsies from hypogonadal men with osteoporosis show a high bone turnover rate, as compared with eugonadal osteoporotic men. In men with Klinefelter's syndrome, those who were treated with testosterone at an early age showed better bone density than those treated when they were older. Men with hyperprolactinemia who were treated showed improvements in the bone density only if the testosterone levels increased.
It is interesting to note that estrogen is necessary for bone strength in men. This has been clearly demonstrated in men who lack aromatase, the enzyme which converts testosterone into estrogen. These men fail to close their epipheses and grow tall, but the bone density is low. Treatment with estrogen reverses the abnormalities.
Ten hypogonadal men were treated with testosterone gel for 24 months. They were evaluated with microMRI (magnetic resonance imaging) of the tibia, which demonstrated improvement in the trabecular architecture, as well as the bone density. An example of the images is shown:
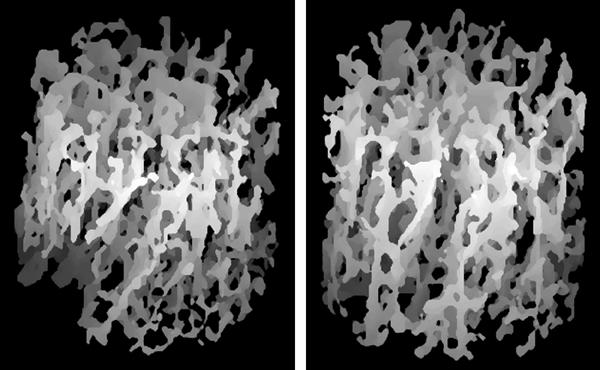
From Benito M. Effect of testosterone replacement on trabecular architecture in hypogonadal men. J Bone Miner Res 2005;20(10):1785-91. Reprinted with permission from the American Society of Bone and Mineral Research
A larger study of 70 men treated for 36 months showed improvement of bone density:
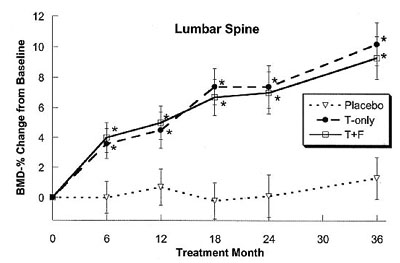
Amory, J. K.(2004). Exogenous testosterone or testosterone with finasteride
increases bone mineral density in older men with low serum testosterone.
J Clin Endocrinol Metab 89: 503-10. ©2004 The Endocrine Society, used with permission.
The following table shows some clinical studies of testosterone therapy on bone density in men. This table is not yet complete, there have been other studies that will be added
| Author | Year | Design | N | Population | ages | Duration | Results |
|---|---|---|---|---|---|---|---|
| Amory | 2004 | RCT | 70 | hypogonadism | 65+ | 3 yrs | spine BMD up 10%, hip up 2.7% |
| Leifke | 1998 | prospective | 32 | hypogonadism | 18-74 | mean 3.2 yrs | significant increase in BMD in all pts |
| Behre | 1997 | prospective | 72 | hypogonadism | 18-74 | mean 2.7 yrs | QCT 95 - 125 |
| Reid | 1996 | cross-over | 15 | asthmatic on glucocorticoids | .. | 1 yr | spine BMD up 5% |
| Anderson | 1996 | prospective | 21 | eugonadal osteoporosis | 34-73 | 6 mo | spine BMD increased 5%, markers decreased |
| Katznelson | 1996 | prospective | 29 | hypogonadal | 22-68 | 18 mo | QCT increased 14%, DEXA up ~6%, markers decreased |
| Hall | 1996 | RCT | 15 | rheumatoid arthritis | 34-79 | 9 mo | spine +1.2% vs -1.1% (NS) |
| Isaia | 1992 | prospective | 6 | hypogonadal | .. | .. | BMD improved |
| Devogelaer | 1992 | prospective | 16 | hypogonadal | .. | .. | radius BMD increased 5.9%/yr |
| Finkelstein | 1989 | prospective | 21 | Gn-RH deficiency | 19-53 | mean 2 yrs | cortical bone at arm increased, QCT spine same or increased in younger men |
Side effects from these studies have not been serious. Reports of increased hemoglobin, decreased HDL, acne, and skin irritation at transdermal sites have been reported. A randomized blinded study of testosterone replacement in hypogonadal men have shown increased grip strength, decreased leptin, and no change in PSA (27). A review of testosterone replacement states that liver abnormalities can be seen but are rare. Breast tenderness and sleep apnea are also seen. There is some debate about changes in lipids and thrombosis. The prostate increases to the size in age-matched controls but does not continue to grow with continuing replacement therapy.
The benefits of reduction in fracture would outweigh these risks. No studies of fracture efficacy have been done. Estimations from studies in women suggest that a 5% increase in bone density should result in about half as many fractures. Testosterone increases muscle mass, which may also reduce fracture risk. Replacement with testosterone is a more physiological approach to osteoporosis treatment than using bisphosphonates. There is no information about combination therapies with testosterone.
Hypogonadal men with non-traumatic fractures and low bone density, or with low bone density and high risk of fractures (for example, on prednisone). It is not clear if bone density should be in reference to other men or to women; I would be concerned about age-and-sex-matched Z scores less than 1.5. There have not been enough studies to recommend this treatment in eugonadal men, although the preliminary data suggests this may be a future choice. Testosterone is contraindicated in men who already have prostate cancer. It should be used with caution in patients on anticoagulants.
Testosterone enanthate or cypionate 200 mg IM Q 2 weeks
Transdermal testosterone patch 5mg daily
Testosterone gel 50mg/5g apply daily
I have not found any consensus about monitoring. It seems reasonable to measure bone density yearly for two or three years; then, if bone mass is stable, the frequency could be reduced (depending on other risk factors). Testosterone levels should be in the mid-normal range one week post injection or while on the patch; I don't check these more often than yearly. Cholesterol, hematocrit, liver function and prostate size should be checked yearly.
Bisphosphonates These have been studied in men with osteoporosis, and the results are beneficial and similar to results in women. In men who have osteoporotic fractures, either testosterone or a bisphosphonate would be the first choices for therapy. The doses and side effects are the same as for women.
Teriparatide (intermittent PTH) This also has been studied in men, and is a choice for somebody with severe osteoporosis who has not responded to other therapies.
Calcitonin This has not been extensively studied in men, but it is reasonable to use this agent in mild cases or as a second choice if side effects prevent other choices.
Thiazides In males, about 20% of otherwise idiopathic osteoporosis is related to hypercalciuria. Small studies have shown that thiazides improve the bone density in these cases, but large fracture studies have not been done. Many epidemiologic prospective studies have demonstrated decreased hip fracture risk in men who have taken thiazides (mostly the indication was hypertension). This drug is not usually recommended primarily for prevention of osteoporosis because the appropriate studies for fracture prevention have never been done (the drug is just too inexpensive for companies to make any profit).
Basically, the treatment for men is the same as for women, except testosterone is used instead of estrogen, and there is not enough data about SERMS to recommend treatment in men.
Reviewed 5/16/2010