
Pleural Effusions
Case 7 Answers
A 65 year-old retired military officer with a history of rheumatoid arthritis presents to clinic with increasing dyspnea. He denies recent fevers, chills, or respiratory infections. His exam reveals dullness to percussion and decreased breath sounds on the right side of his chest, extending two-thirds of the way up his back so you order a chest x-ray which confirms the presence of a right pleural effusion. A thoracentesis is performed and you draw out fluid, a sample of which is shown below:

What diagnoses should you consider based on the appearance of the pleural fluid?
This fluid has a milky appearance. The two primary items to consider on the differential diagnosis when you see this are chylothorax (chyle or lymph fluid in the pleural space due to disruption of the thoracic duct) and pseudochylothorax (some chronic inflammatory process, such as rheumatoid pleurisy, leads to the deposition of cholesterol crystals in the pleural space). Cloudy fluid also raises the possibility of empyema but the clinical history in this case is not suggestive of this process.
You should be aware that the milky appearance in chylothorax is due to the presence of chylomicrons in the pleural fluid. If patients are malnourished or are taking in a diet very low in triglycerides, they do not generate chylomicrons and the pleural fluid may not have the classic milky appearance even though they still have a disruption of their thoracic duct and chylothorax.
The pleural fluid analysis shows LDH 567 (serum value 200), with a total protein of 4.6 (serum value 7.2). The gram’s stain has white cells but no organisms. The WBC differential includes 80% lymphocytes, 15% monocytes and 3% polymorphonuclear cells.
How do you interpret the results of the pleural fluid analysis?
The LDH is greater than the upper limit of normal for serum and the pleural fluid: serum ratio for LDH is > 0.6 while the pleural fluid: serum ratio for protein is > 0.5. This effusion, therefore, should be classified as an exudative process. The fluid contains 80% lymphocytes and, therefore, this should be classified as a lymphocyte-rich pleural effusion. As noted earlier, the leading items on the differential for such effusions includes tuberculous pleurisy, lymphoma, chylothorax, chronic rheumatoid pleurisy, sarcoidosis and some other less common causes.
What additional studies should you order at this time?
Given that you aspirated milky fluid and have a lymphocyte-rich pleural effusion, chylothorax should be high on the differential diagnosis. This diagnosis is confirmed by ordering a triglcyeride level on the pleural fluid. Because he has chronic rheumatoid arthritis you would consider rheumatoid pleurisy and order a rheumatoid factor on the pleural fluid. You would also have to consider the possibility of a pseudochylothorax, which can occur in the setting of chronic rheumatoid pleurisy. To rule out this possibility you should order a total cholesterol level on the pleural fluid.
The triglyceride level in the pleural fluid comes back at 160 mg/dL. Cholesterol level is 150 mg/dL. How do you interpret these results?
In chylothorax, the triglyceride level in the pleural fluid will be > 110 mg/dL and the cholesterol level is < 200 mg/dL while in pseudochylothorax, the triglyceride level is < 50 mg/dL and the cholesterol level is > 200 mg/dL. His studies are, therefore, consistent with this being a chylothorax
What is the next most appropriate study for you to order on this patient?
Chylothorax occurs as a result of disruption of the thoracic duct. The majority of cases (~70%) are non-traumatic, while the remaining cases occur as the result of traumatic injuries such as surgical complications or blunt chest trauma. In cases of non-traumatic chylothorax, the overwhelming majority of cases are due to lymphoma. Because this patient did not have a history of recent chest trauma, you need to consider lymphoma on the differential until proven otherwise and should obtain a CT scan of the chest to investigate this possibility.
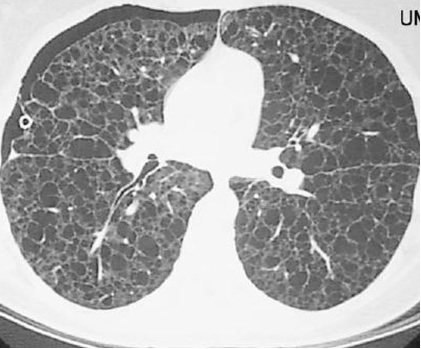
Suppose this patient had been a 30 year-old woman with a history of recurrent pneumothoraces and a CT scan similar to the one shown below. What diagnosis would you consider in this case?
Recurrent spontaneous pneumothoraces in women of child-bearing age should raise the possibility of two different diagnoses: catamenial pneumothorax due to the presence of endometrial tissue on the pleural surfaces, and lymphangioleiyomyomatosis, a disorder marked by abnormal smooth muscle proliferation in the lungs. The CT scan shows evidence of diffuse cystic lung disease, the hallmark of advanced lymphangioleiyomyomatosis, also referred to as LAM. This disorder can be associated with the development of chylothorax because the smooth muscle proliferation interferes with lymphatic drainage from the lungs.
UW School of Medicine : School of Medicine Mission
Copyright and Disclaimer : Credits and Acknowledgements