Pleural Effusions
Case 8 Answers
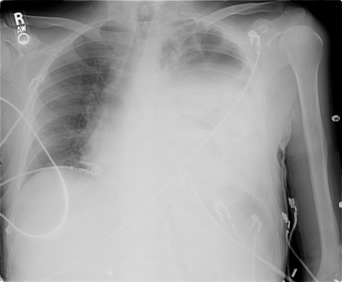
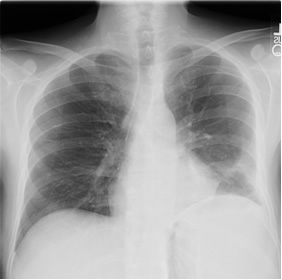
A 45 year-old man is seen in clinic for fever, productive cough and dyspnea on exertion of several days duration. A chest x-ray shown below (top film) revealed a left lower lobe pneumonia but he was deemed stable for outpatient treatment and was sent home on oral levofloxacin. Two days later, he returns complaining of increasing fevers, worsening left-sided chest pain and increasing dyspnea. A chest x-ray is obtained and is shown below (bottom film):
How would you interpret the chest x-rays?
The top chest x-ray shows a subtle left lower lobe opacity just lateral to the heart. In the repeat film several days later, there is a dense opacity over most of the left chest that obscure the left hemidiaphragm and the left hear border. Although there is no clear meniscus , the dense, homogeneous appearance of the opacity as well as the fact that it came up over just a few days strongly suggests that this is an effusion.
What should be your next step in the work-up?
In the setting of a patient who has had symptoms and a chest x-ray compatible with pneumonia, the presence of a new effusion in a patient with worsening fevers, chest pain and dyspnea should raise a strong suspicion for a parapneumonic effusion or empyema. You will need to do a prompt thoracentesis to investigate this possibility. Although the effusion is large and you might think you could do the procedure safely without further imaging, either lateral decubitus films or an ultrasound to mark the fluid collection are warranted. Parapneumonic effusions can go from being free-flowing fluid collections to loculated effusions in a short period of time and you would want to make sure you were putting your needle into the proper space.
You do the appropriate diagnostic study and then perform a thoracentesis. The pleural fluid is cloudy appearing. Pleural fluid LDH is 1050 (serum value 135) with a total protein of 4.8 (serum value 7.8). Gram’s stain reveals 3+ WBC with gram positive cocci in chains. The WBC differential includes 75% polymorphonuclear cells, and 20% monocytes. The pH of the pleural fluid is 7.15 and the pleural fluid glucose is 25.
How do you interpret these results?
The LDH is greater than the upper limit of normal for serum; the pleural fluid: serum ratio for LDH is > 0.6 while the pleural fluid: serum ratio for protein is > 0.5. This effusion, therefore, should be classified as an exudative process. More importantly, the gram’s stain has evidence of gram positive cocci. The patient, therefore, has an infected pleural space. Depending on which source you read, this may or may not be called an empyema. Some sources reserve the term empyema for pus in the pleural space while other sources will use the term to describe either pus in the pleural space or fluid with organisms on gram’s stain and/or culture
How do you interpret the pleural fluid pH and pleural fluid glucose?
Glucose values greater than 60 in the pleural space are considered unremarkable. Low glucose values have some diagnostic utility as values between 30 and 50 are seen in tuberculous pleurisy, lupus pleuritis, malignancy and esophageal rupture while values below 30 are seen in empyema, Tb empyema and rheumatoid pleurisy. Most transudates have pH values between 7.40 and 7.55 while most exudates have values between 7.30 and 7.45. pH values below 7.30 have the same differential diagnosis as low glucose values. In this particular case, the low glucose and low pH values are consistent with the diagnosis you have already made by other means so they do not add much value to the work-up. The American College of Chest Physicians (ACCP) has consensus guidelines for the management of parapneumonic effusions in which pH values below 7.21 are seen as an indication to drain the effusion but this recommendation is based on weak data.
What is the next most appropriate management step for this patient? For what problem is this patient at risk if you fail to take the appropriate action in this case?
Because the patient has an infected pleural space, this fluid should be drained promptly. There is a lot of debate as to the proper drainage procedure. Some people argue that it is okay to start with tube thoracostomy (chest tube) and proceed to a surgical procedure if they don’t respond while others claim that it is best to do a video-assisted thoracoscopic surgery from the outset instead of a chest tube. Proponents of the latter position claim that the effusion has a high likelihood of becoming loculated and creating a complicated pleural space if it not drained promptly. Chest tubes merely delay the time to a definitive treatment procedure. Unfortunately, there is not a lot of data to mediate this debate and decisions are individualized based on the details of the patient’s clinical condition and who the consulting surgeon is for that day.
Failure to drain the effusion by any means can have severe consequences for the patient. The effusion can become loculated and the patient may develop a fibrous peel around the lung which will eventually necessitate a more difficult surgical procedure than if it had been drained at an earlier stage.
UW School of Medicine : School of Medicine Mission
Copyright and Disclaimer : Credits and Acknowledgements