
Pleural Effusions
Case 9 Answers
A 55 year-old woman underwent thoracotomy for a resection of a posterior mediastinal mass. She had a right subclavian line placed, which was working properly. She has not been eating well since the surgery and has been on maintenance fluid with half-normal saline. Her chest tube was removed on post-operative day #1. Two days later she developed dyspnea, hypoxemia and a headache that was worse in the upright position. A chest x-ray was performed and showed a large right pleural effusion. Thoracentesis is performed and reveals clear “water-like” fluid. The LDH is 80 (serum value 190) and the total protein is < 1 (serum value 6.9). There are no WBCs and the gram’s stain is negative. The WBC differential contains primarily monocytes.
How do you interpret the pleural fluid results?
The LDH is less than 2/3 of the upper limit of normal for serum with a pleural fluid: serum ratio of 0.42. The pleural fluid: serum ratio for protein is 0.14. This fluid is, therefore, consistent with a transudative process.
What is the differential diagnosis for colorless pleural fluid with a total protein < 1?
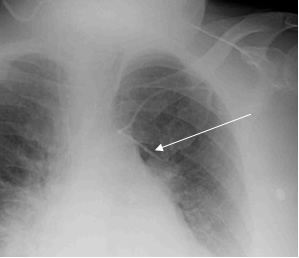
Colorless pleural fluid with a total protein < 1 is only seen in a small number of circumstances including duro-pleural fistulas, urinothorax, peritoneal dialysis patients and patients in who intravascular catheters migrate through the vessel wall into the thoracic cavity. In this particular case, you should consider migration of a central venous catheter and duro-pleural fistula as the two most likely causes. She has a central venous catheter from the time of her surgery and the particular procedure, a thoracic surgery with operative work near the spinal column, increases the risk for puncturing the dura and creating a communication between the subarachnoid and pleural spaces. An x-ray from another patient whose intravascular catheter has migrated into the thoracic cavity is shown below.
Because her catheter had been functioning well to this point, the likelihood of the catheter tip migration is low.
In addition to ordering an LDH and protein level on the pleural fluid, what additional diagnostic studies should you consider to confirm the diagnosis?
The diagnosis of duro-pleural fistula can be confirmed by checking a beta-transferrin level on the pleural fluid. This substance is seen in CSF but not other bodily fluids. Therefore, its presence in the pleural fluid is confirmation of a communication between the subarachnoid and pleural spaces.
UW School of Medicine : School of Medicine Mission
Copyright and Disclaimer : Credits and Acknowledgements