
Pleural Effusions
Case 7
A 65 year-old retired military officer with a history of rheumatoid arthritis presents to clinic with increasing dyspnea. He denies recent fevers, chills, or respiratory infections. His exam reveals dullness to percussion and decreased breath sounds on the right side of his chest, extending two-thirds of the way up his back so you order a chest x-ray which confirms the presence of a right pleural effusion. A thoracentesis is performed and you draw out fluid, a sample of which is shown below:

What diagnoses should you consider based on the appearance of the pleural fluid?
The pleural fluid analysis shows LDH 567 (serum value 200), with a total protein of 4.6 (serum value 7.2). The gram’s stain has white cells but no organisms. The WBC differential includes 80% lymphocytes, 15% monocytes and 3% polymorphonuclear cells.
How do you interpret the results of the pleural fluid analysis?
What additional studies should you order at this time?
The triglyceride level in the pleural fluid comes back at 160 mg/dL. Cholesterol level is 150 mg/dL. How do you interpret these results?
What is the next most appropriate study for you to order on this patient?
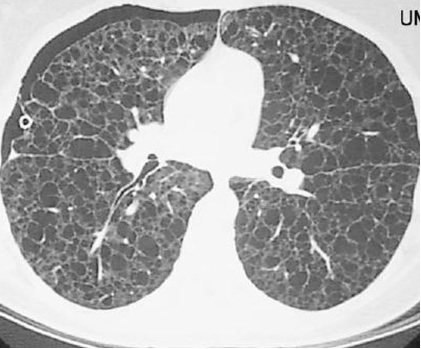
Suppose this patient had been a 30 year-old woman with a history of recurrent pneumothoraces and a CT scan similar to the one shown below. What diagnosis would you consider in this case?
UW School of Medicine : School of Medicine Mission
Copyright and Disclaimer : Credits and Acknowledgements