When to add medications
Physicians must pay attention to basic prevention before writing a prescription. Medications do not work as well (if at all) in patients who have poor nutrition, vitamin D deficiency, or lack of exercise. In frail women and men, fall prevention should be part of the plan. Patients with secondary osteoporosis may require different treatments from those that are useful for primary osteoporosis.
Addition of pharmaceutical treatment should be based on the risk of fractures. Using the bone density, age, presence of fracture, other risk factors, and general health, a risk of fracture can be estimated, using the Fracture Risk Calculator.These risks have been derived from observations of over 100,000 people world-wide, so they are fairly accurate.
 Treatment decisions can not be made from fracture risk alone, but depend on the cost, effectiveness, and safety of the treatments! For example, a rodeo rider has a high risk of fracture, which will not be improved with Fosamax.
There is disagreement about the threshold that should be used to decide about starting treatment.
Treatment decisions can not be made from fracture risk alone, but depend on the cost, effectiveness, and safety of the treatments! For example, a rodeo rider has a high risk of fracture, which will not be improved with Fosamax.
There is disagreement about the threshold that should be used to decide about starting treatment.
A cost-effective analysis (Tosteson) suggests that treatment is beneficial when the risk of a hip fracture in the next ten years is greater than 3%. This analysis made optimistic assumptions about the effectiveness and long-term safety of the drugs. Another analysis, by Kanis, finds a cost-effectiveness threshold that ranges from 1.1% at age 50 to 9% at age 85. A report by
Schousboe found that alendronate is not cost-effective in treating women unless the T-score was lower than -2.5 or they already had an adult fracture.
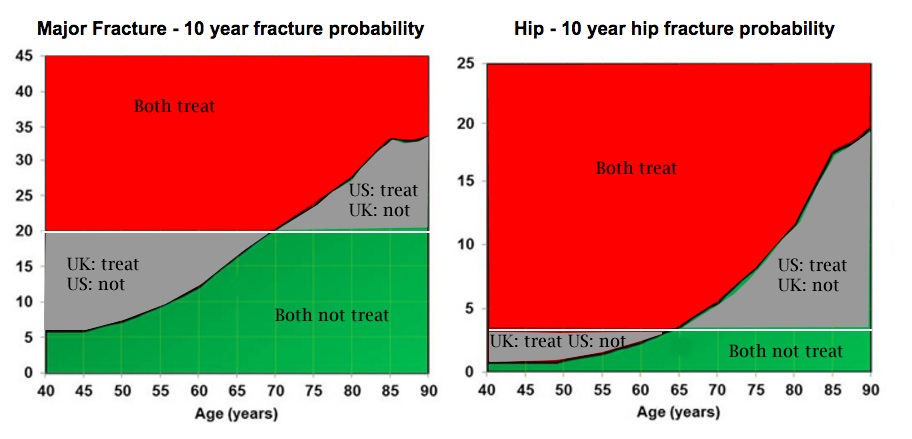
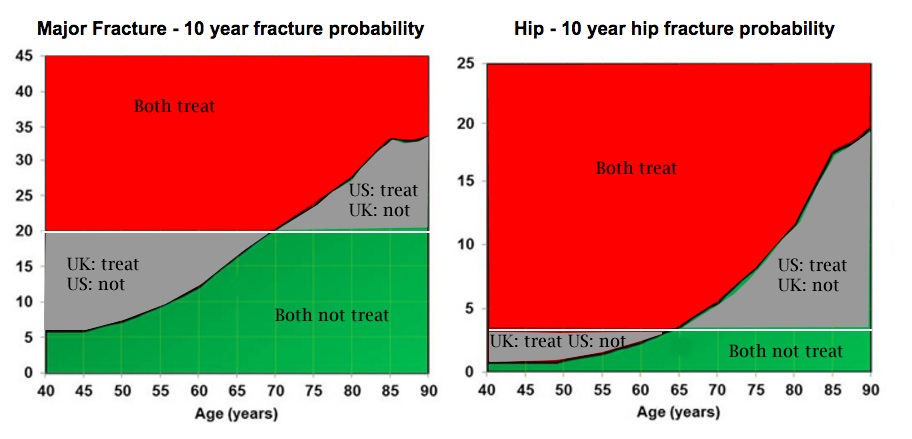
The graph is modified from the National Osteoporosis Guideline Group in the UK, and is from the FRAX website. The white lines represent the views of the National Osteoporosis Foundation in the US (Dawson-Hughes), who recommend treatment above a 10-year hip fracture risk of 3% or a major fracture risk of 20%. The red regions and green regions show fracture risks when both the USA and the UK agree on treatment, and the grey regions show where they disagree.
A study in men showed that the NOF guidelines would have resulted in treating a large percentage of men who would not experience a fracture. The authors thought it was unlikely to see a benefit of treatment (using the current medications) in men with an increased fracture risk unless the hip T-scores was lower than -2.5 (Ensrud, 2014).
If the NOF guidelines were used, then almost all white women over the age of 75 would be treated, as shown in a paper by Donaldson MG using data from the Study of Osteoporotic Fractures. These authors suggest that more studies on the effectiveness and safety of the medications should be done before such wide-spread use is advocated. Another study using data from NHANES (Dawson-Hughes) found similar numbers, as shown in the following graph. The impact of age is also seen in the NHANES analysis.

Some examples
Disagreements are because the current studies don't give clear answers. They demonstrate how important it is for more research. Here are some examples of what I would do (sometimes if a patient can't tolerate these choices I suggest calcitonin). I want to stress the fact that every patient has to be treated on an INDIVIDUAL basis, and what works for one may not be best for another.
Risk of hip fracture
in 10 yr
| Example
(T-score at hip)
| Drug choices
in addition to basic prevention
|
| Below 1% | Young strong woman, no risks | none
|
| Below 3% | Young woman with "osteopenia", no risks | wait until menopause for treatment
|
|---|
| 1.5% | Early postmenopausal woman, T-score -2, no other risks | uncertain, see choices
|
|---|
| 1.7% | 68 yr old woman, osteopenia (T-score -2, no risks) | none
|
|---|
| 4.6% | Healthy 67 yr old woman, T-score -2.8, no other risks or fractures | raloxifene, bisphosphonate
|
|---|
| 4.7% | 68 yr old woman, T-score -2.2, smoker, BMI 20 | stop smoking, increase calories
|
|---|
| 9.9% | 72 yr old woman with T-score -2.8 and vertebral fracture | bisphosphonate, raloxifene
|
|---|
| 5% | 70 yr old woman, no fractures, breast cancer on letrozole | denosumab, bisphosphonate
|
|---|
| 3% | 85 yr old woman with T-score -1.5, no risks | none
|
|---|
| 2.6% | 55 yr old man with hypogonadism, Z-score -1.9 | testosterone
|
|---|
| 1.5% | 50 yr old man with kidney stone, hypercalciuria, Z-score -1.5 | thiazide
|
|---|
| 7-9% | 65 yr old woman or man with T-score -3 with vertebral fracture while on treatment | teriparatide
|
|---|
| High | Patient with liver transplant | specialized treatment
|
|---|
| High | 52 yr old woman with chronic kidney disease stage 5 | raloxifene, avoid bisphosphonate
|
|---|
| High | Patient with hypocalcemia and intestinal bypass | calcitriol
|
|---|
| High | Premenopausal woman taking steroids | individualize treatment
|
|---|
Comments
| Women or men with hip or vertebral fractures need therapy | Medical treatment should be given to prevent further bone loss and to reduce the risk of more fractures. These patients are at high risk and they benefit from potent medications. With the information available today, there is no excuse to ignore this condition. The high short-term risk outweighs the potential long-term side effects of treatment. Be sure to check for secondary causes, not all the fractures are due to osteoporosis.
|
| Bisphosphonates | Bisphosphonates have been approved by the FDA for prevention of osteoporosis, and they are widely used in women younger than 65. However, I am reluctant to use them in young or low-risk women, and reserve these drugs for those with established osteoporosis. I have a more conservative view about long-term safety issues than many other physicians, perhaps because I have a physiological perspective. Bone biopsies from patients taking bisphosphonates show 95% reduction in the bone formation rate, so I usually stop after 5 years of treatment.
The bisphosphonates get deposited in the bone and will accumulate for years. More than 5 years of continuous medicine can make bone brittle or impair the ability to repair damage. Bisphosphonates do reduce fractures and improve measurements of bone strength for the first five years in both animal studies and in women who have osteoporosis. After 5 years, there is enough bisphosphonate in the bone to last for the next 5 years and it is usually best to stop.
|
| Other anti-resorbing agents | Estrogen, calcitonin, and raloxifene also are anti-resorbing medicines. They do not accumulate, and on bone biopsies the bone formation is similar to pre-menopausal levels. Estrogen has been shown to continually maintain bone strength for 30 years - it is the only medication with such a long track record. Estrogen also has been shown to prevent osteoporotic fractures, including hip fractures, in a large randomized study. However, if combination hormones (estrogen plus progestin) are started in women ten or more years beyond menopause there is an increased risk of heart disease and breast cancer. In women older than 60 who are started on estrogen only (no progestin) there was no increased risk of heart disease or breast cancer but there were more strokes. These risks were not seen in women who were within ten years of menopause. I think it is still reasonable to use estrogen in perimenopausal women (within 5 years of menopause). The duration of estrogen use is uncertain; in the past women used estrogen into their 80's and had fewer fractures and fewer heart attacks.
|
| Healthy premenopausal women | I do not recommend any drug therapy, even if they have osteopenia (remember, by definition 16% of 25-year-old women have osteopenia). Nothing has been shown to be effective, and all drugs have risks. These young women should get calcium and exercise and avoid weight loss. However, if they have amenorrhea or oligomenorrhea they need estrogen, such as birth control pills with 20 mcg of estinyl estradiol. Depo-provera appears to enhance bone loss and should be avoided in women with high risk of osteoporosis.
Bisphosphonates should NOT be given to women who are planning to get pregnant.
|
| Diagnosis | Before beginning treatment, a diagnostic workup should be done to be sure that the disease is primary osteoporosis. Patients with secondary osteoporosis may require more specific therapy.
|
| Follow-up | Whichever treatment is chosen, physicians should be aware that follow-up bone density tests are not completely reproducible. Even a slight loss of bone density could represent an acutal gain, and could mean that the patient was responding. Repeating the bone density in a year can give a longer-term picture. In cases of high risk, bone markers might help to decide if the therapy is working when the bone density is borderline.
|
Updated 2/25/16


 Treatment decisions can not be made from fracture risk alone, but depend on the cost, effectiveness, and safety of the treatments! For example, a rodeo rider has a high risk of fracture, which will not be improved with Fosamax.
There is disagreement about the threshold that should be used to decide about starting treatment.
Treatment decisions can not be made from fracture risk alone, but depend on the cost, effectiveness, and safety of the treatments! For example, a rodeo rider has a high risk of fracture, which will not be improved with Fosamax.
There is disagreement about the threshold that should be used to decide about starting treatment.